The consumption of alcohol is one of the most common forms of substance use worldwide, with profound neuropsychological implications. In this article, psychologist Rafael A. Salas Muriel explains, from a neuropsychological perspective, what alcohol is, its effects on the brain, the risks associated with its consumption, and how neuropsychological assessment and intervention can contribute to the treatment of people affected by this type of consumption.
What is alcohol?
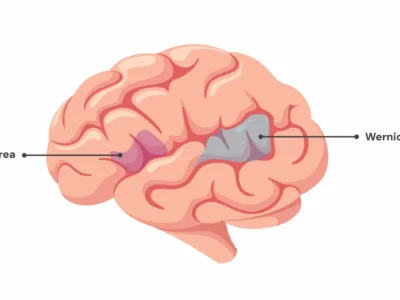
Ethanol, commonly known as alcohol, is a psychoactive substance that acts as a depressant of the central nervous system. When consumed, it crosses the blood-brain barrier and affects various areas of the brain, particularly those associated with motor control, judgment and decision-making (Waisman and Benabarre, 2021).
Chronic alcohol consumption can lead to a range of neurological disorders, with consequent cognitive and psychological deficits due to its impact on brain structures.
Neuropsychological alterations associated with alcohol consumption
Prolonged and excessive alcohol consumption can produce multiple neuropsychological alterations, especially in those who develop alcohol dependence (Courtney et al., 2019). Below are some of the main neuropsychological effects that can be observed in people who consume alcohol chronically:
1. Memory impairment
Alcohol significantly affects the memory, particularly the ability to form new memories. The hippocampus, a key brain structure for storing information, is affected, leading to difficulties remembering recent events. In cases of chronic abuse, people may develop Korsakoff syndrome, characterized by severe amnesia and confabulation (Akhouri et al., 2023).
2. Attention deficit
People who consume alcohol may have difficulty concentrating and filtering out irrelevant stimuli, affecting their ability to stay focused on specific tasks (Cabé et al., 2018). In the long term, these attentional deficits can seriously compromise performance in everyday tasks and work contexts.
3. Executive dysfunction
The executive functions, such as decision-making, planning and impulse control, are particularly sensitive to excessive alcohol consumption. People with alcohol dependence may exhibit impulsive behaviors, difficulty organizing themselves and making appropriate decisions (McPhee and Hendershot, 2023), which can severely affect their personal and professional lives.
4. Emotional alterations
Alcohol can produce significant changes in emotional regulation, leading to states of euphoria or, conversely, episodes of depression and anxiety. People who abuse alcohol often present a greater vulnerability to affective disorders (McHugh and Weiss, 2019), due to its effect on neurotransmission systems.
5. Thought disorders
Chronic alcohol consumption can induce disorganized thoughts and difficulties following a coherent line of thinking. In severe cases, people may develop delirium tremens or psychotic episodes, characterized by hallucinations and confusion.
It is necessary to remember that acute conditions such as delirium tremens, produced by abrupt withdrawal when there has been high alcohol consumption (Rahman and Paul, 2023), can lead to death if not properly treated in a hospital setting.
6. Reduced processing speed
Alcohol can slow the brain’s ability to process information, negatively affecting the ability to respond quickly to stimuli (Czapla et al., 2016). This is especially problematic in situations such as driving, where reaction speed is crucial.
7. Impact on motivation
Like other substances, alcohol can reduce motivation to engage in activities that were previously rewarding. People who abuse alcohol may experience apathy, lack of energy and difficulties initiating and completing tasks (Pavkovic et al., 2018), which significantly affects their quality of life.
Neuropsychological assessment
Neuropsychological assessment in patients with alcohol use is essential to identify and quantify the cognitive and emotional deficits associated. This process begins with a detailed clinical interview to explore the history of consumption, current symptoms and the impact on the patient’s daily life. Next, various neuropsychological tests that assess key cognitive functions are administered.
Among the most commonly used tests is the Stroop Test, which measures inhibitory control and attentional capacity, and the Spain-Complutense Verbal Learning Test (TAVEC), which evaluates verbal memory and learning. These tests help neuropsychologists obtain a detailed cognitive profile of the patient, identifying areas affected by alcohol consumption.
Another commonly used set of tests is the Halstead-Reitan Neuropsychological Battery, which evaluates cognitive flexibility, processing speed and abstract reasoning. In addition, the Trail Making Test, which assesses attention and executive function, and the Wisconsin Card Sorting Test (WCST), which measures the ability to adapt to new patterns or rules, can be employed.
Neuropsychological assessment is essential not only to identify deficits but also to guide personalized interventions that help patients rehabilitate their affected cognitive functions.

Subscribe
to our
Newsletter
Neuropsychological intervention
Neuropsychological intervention in patients with alcohol use focuses on rehabilitating deteriorated cognitive functions through strategies of cognitive rehabilitation and cognitive-behavioral therapy (CBT). Cognitive rehabilitation includes exercises designed to improve memory, attention and executive functions.
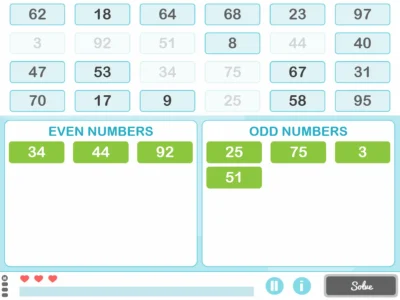
In this regard, NeuronUP is especially useful for addressing deficits in areas such as memory, attention and executive functions, which are often severely affected by chronic consumption of this substance. By providing personalized exercises adapted to the individual needs of each patient, this tool allows systematic and progressive work on cognitive recovery, facilitating improvements in specific skills such as planning, decision-making and impulse control.
In addition, NeuronUP allows neuropsychologists to monitor the patient’s progress in detail over time. This is fundamental in the treatment of alcoholism, since the neuropsychological effects of alcohol can vary significantly from one patient to another. The platform offers constant feedback, allowing the exercises to be adjusted and adapted according to the evolution of the patient’s cognitive abilities. In this way, NeuronUP not only optimizes neuropsychological intervention but also increases the chances of long-term success, improving patients’ quality of life and their functional reintegration into social and work environments.
On the other hand, cognitive-behavioral therapy is a complementary tool that helps patients identify thought and behavior patterns related to alcohol use. CBT teaches strategies to control urges to drink and manage stress, which facilitates abstinence and improves quality of life (Cohen et al., 2022).
Another important component of the intervention is psychoeducation, where the patient is educated about the effects of alcohol on their brain and how to manage triggering factors that may lead to consumption. Family intervention can also play a key role, offering support to the patient and improving family dynamics through therapy. It is very important to have the support of the patient’s close contacts, especially in cases of chronic abuse.
To illustrate everything described about the neuropsychology of alcohol, a clinical case example is presented below.
Clinical case
A 45-year-old man with a history of chronic alcohol consumption since the age of 25 attended the clinic. Despite having attempted to reduce his consumption on several occasions, he has been in a situation of severe dependence for the past five years, presenting episodes of intensive consumption, mainly during stressful situations. What most prompts him to seek help is that he perceives some difficulties in his day-to-day life. He reports difficulties remembering where he has placed some objects, as well as intense irritability when something does not go as he wishes. He also describes other situations that cause clinically significant distress in his daily life.
During the neuropsychological assessment, significant deficits were identified in short-term memory and in executive functions, such as planning and decision-making. The patient showed difficulties recalling recent events, as well as problems organizing his day-to-day life and meeting work responsibilities. Regarding his emotions, he alternated between states of anxiety and depression, which exacerbated his alcohol use as a coping method.
Tests such as the Stroop Test were applied, where he showed reduced inhibitory control, and the TAVEC, which confirmed problems in the consolidation of verbal memory. In the Trail Making Test, he showed a notably decreased processing speed.
The intervention plan included a program of cognitive rehabilitation with exercises to improve memory and executive function. All exercises were carried out through the NeuronUP platform, through several weekly sessions, some of which, as treatment progressed, were carried out from the patient’s home. The patient’s progress was then monitored thanks to the graphs that NeuronUP displayed on its platform.
In parallel, cognitive-behavioral therapy was implemented to help him manage stress and reduce craving, complemented with sessions of psychoeducation about the effects of alcohol on his brain and relapse prevention strategies (Harada et al., 2016). A pharmacological treatment was also initiated with Psychiatry to support the maintenance of alcohol abstinence.
Future perspectives and research
Future perspectives in the neuropsychology of alcohol focus on a greater understanding of the neurobiological mechanisms underlying the effects of chronic alcohol consumption on the brain. Current research is exploring how alcohol-induced brain damage, such as cortical atrophy and alterations in neuronal circuits, affects critical cognitive functions such as memory and executive function (Egervari et al., 2021). It is expected that advances in neuroimaging and neuromodulation techniques, such as transcranial magnetic stimulation (TMS), may offer a more precise view of the impact of alcohol on specific brain structures and open new avenues for more personalized treatments based on neuroplasticity (Diana et al., 2019; Fein and Cardenas, 2015), facilitating cognitive rehabilitation more effectively.
On the other hand, future research in the neuropsychology of alcohol is also moving toward multidisciplinary approaches that combine neuropsychological treatments with more advanced pharmacological therapies. For example, drugs are being developed that could protect the brain from the neurotoxic effects of alcohol or even reverse some of the damage (Witkiewitz et al., 2019). At the same time, combined digital therapeutic approaches are being studied, such as mobile apps that integrate behavioral and neuropsychological interventions (Staiger et al., 2020).
These innovations have the potential to improve accessibility to high-quality treatments, offering continuous rehabilitation outside traditional clinical settings and increasing the chances of sustained recovery.
Bibliography
- Akhouri, S., Kuhn, J., & Newton, E. J. (2023). Wernicke-Korsakoff Syndrome. In StatPearls. StatPearls Publishing.
- Cabé, N., Laniepce, A., Boudehent, C., Pitel, A. L., & Vabret, F. (2018). Atteintes cognitives liées au trouble de l’usage d’alcool: rétablir l’équilibre ? [Cognitive impairment]. Presse medicale (Paris, France: 1983), 47(6), 565–574. https://doi.org/10.1016/j.lpm.2018.01.017
- Cohen, S. M., Alexander, R. S., & Holt, S. R. (2022). The Spectrum of Alcohol Use: Epidemiology, Diagnosis, and Treatment. The Medical clinics of North America, 106(1), 43–60. https://doi.org/10.1016/j.mcna.2021.08.003
- Courtney, K. E., Li, I., & Tapert, S. F. (2019). The effect of alcohol use on neuroimaging correlates of cognitive and emotional processing in human adolescence. Neuropsychology, 33(6), 781–794. https://doi.org/10.1037/neu0000555
- Czapla, M., Simon, J. J., Richter, B., Kluge, M., Friederich, H. C., Herpertz, S., Mann, K., Herpertz, S. C., & Loeber, S. (2016). The impact of cognitive impairment and impulsivity on relapse of alcohol-dependent patients: implications for psychotherapeutic treatment. Addiction biology, 21(4), 873–884. https://doi.org/10.1111/adb.12229
- Diana, M., Bolloni, C., Antonelli, M., Di Giuda, D., Cocciolillo, F., Fattore, L., & Addolorato, G. (2019). Repetitive transcranial magnetic stimulation: Re-wiring the alcoholic human brain. Alcohol (Fayetteville, N.Y.), 74, 113–124. https://doi.org/10.1016/j.alcohol.2018.05.011
- Egervari, G., Siciliano, C. A., Whiteley, E. L., & Ron, D. (2021). Alcohol and the brain: from genes to circuits. Trends in neurosciences, 44(12), 1004–1015. https://doi.org/10.1016/j.tins.2021.09.006
- Fein, G., & Cardenas, V. A. (2015). Neuroplasticity in Human Alcoholism: Studies of Extended Abstinence with Potential Treatment Implications. Alcohol research : current reviews, 37(1), 125–141.
- Harada, T., Aikawa, Y., Takahama, M., Yumoto, Y., Umeno, M., Hasegawa, Y., Ohsawa, S., & Asukai, N. (2022). A 12-session relapse prevention program vs psychoeducation in the treatment of Japanese alcoholic patients: A randomized controlled trial. Neuropsychopharmacology reports, 42(2), 205–212. https://doi.org/10.1002/npr2.12248
- McHugh, R. K., & Weiss, R. D. (2019). Alcohol Use Disorder and Depressive Disorders. Alcohol research: current reviews, 40(1), arcr.v40.1.01. https://doi.org/10.35946/arcr.v40.1.01
- McPhee, M. D., & Hendershot, C. S. (2023). Meta-analysis of acute alcohol effects on response inhibition. Neuroscience and biobehavioral reviews, 152, 105274. https://doi.org/10.1016/j.neubiorev.2023.105274
- Pavkovic, B., Zaric, M., Markovic, M., Klacar, M., Huljic, A., & Caricic, A. (2018). Double screening for dual disorder, alcoholism and depression. Psychiatry research, 270, 483–489. https://doi.org/10.1016/j.psychres.2018.10.013
- Rahman, A., & Paul, M. (2023). Delirium Tremens. In StatPearls. StatPearls Publishing.
- Staiger, P. K., O’Donnell, R., Liknaitzky, P., Bush, R., & Milward, J. (2020). Mobile Apps to Reduce Tobacco, Alcohol, and Illicit Drug Use: Systematic Review of the First Decade. Journal of medical Internet research, 22(11), e17156. https://doi.org/10.2196/17156
- Waisman, M., and Benabarre, A. (2021). Adicciones: Uso de sustancias psicoactivas y presentaciones clínicas de la enfermedad adictiva. Editorial Médica Panamericana.
- Witkiewitz, K., Litten, R. Z., & Leggio, L. (2019). Advances in the science and treatment of alcohol use disorder. Science advances, 5(9), eaax4043. https://doi.org/10.1126/sciadv.aax4043
If you liked this article about the neuropsychology of alcohol, you will surely be interested in these NeuronUP articles:
“This article has been translated. Link to the original article in Spanish:”
Neuropsicología del alcohol



 Discover the 10 NeuronUP activities most commonly used for working with adults
Discover the 10 NeuronUP activities most commonly used for working with adults
Leave a Reply