In this post, psychologist and international expert in Alzheimer’s and other dementias, Cristian Francisco Liébanas Vega, talks to us about prematurity and neuropsychological rehabilitation in preterm infants.
Prematurity constitutes a serious problem for both the newborn (NB) and their family, as it is associated with high morbidity at birth and a high risk of future disabilities. The number of children born prematurely and their survival have increased significantly in recent decades due to advances in obstetric and neonatal care. Reducing mortality without increasing morbidity and sequelae is one of the most important challenges in Perinatal Medicine (Rodrigo et al., 2014).
A preterm or preterm birth is defined when delivery occurs before 37 weeks of gestation.
Prematurity can be classified into different groups according to the gestational age at which this birth occurs, or according to the neonate’s weight, since both parameters are usually related in these children. The lower the gestational age and the lower the birth weight, the greater the likelihood of complications derived from prematurity, the higher the risk of death and of sequelae in neurodevelopment.
There are some variables to make classifications within prematurity, such as gestational age or birth weight. According to gestational age, preterm newborns (PNB) are classified as follows:
- Late preterm: birth occurring between 34+0 and 36+6 weeks.
- Moderately preterm: born between 32+0 and 33+6 weeks.
- Very preterm: born between 28+0 and 31+6 weeks.
- Extremely preterm: born before 28 weeks.
According to birth weight, the PNB is classified as follows:
- Low birth weight: weight less than 2500 grams.
- Very low birth weight: weight between 1000 and 1500 grams.
- Extremely low birth weight: weight between 800 and 1000 grams.
- Very extremely low weight: weight less than 800 grams.
It is also important to highlight the concept of weight relative to gestational age. A newborn with low weight for gestational age is one whose birth weight is < the P10 for gestational age and sex. That is, a newborn can be preterm (< 37 weeks), at term (37 to 41 weeks 6 days) or post-term (≥ 42 weeks) and be low weight (< P10), of appropriate weight (PIO-P90) or high weight (> P90) for their gestational age.
A newborn with a birth weight equal to or <1500 g, with gestational age equal to or < 32 weeks and low weight for gestational age are considered neuro-psycho-sensory risk newborns, with a greater possibility of sequelae in their neurodevelopment and will require neuromaturational follow-up at least until 6 years of age within the scope of early intervention (Federación Estatal de Asociaciones de Profesionales de Atención Temprana, 2005) and also later monitoring of executive functions, school learning pace, motor coordination, adaptive skills and behavior, at least in middle childhood and adolescence.
Epidemiology and etiopathogenesis
According to World Health Organization (WHO) sources (Liu et al., 2016), about 15 million preterm babies are born worldwide each year, with prematurity rates varying between 5% and 18%, and in Spain and neighboring countries being around 7% to 9% of all births. Approximately 10% of this group corresponds to PNBs of less than 32 weeks and less than 1500 grams, who concentrate the highest incidence of mortality, morbidity and sequelae throughout their development (Ponte et al., 2022). The late preterm group (34 weeks to 36+6) is the most numerous (70-74% of total PNBs) and although a high percentage will not require admission, they still present a higher risk of complications and sequelae during development than a term newborn (Liu et al., 2016).
A large number of factors intervene in the etiopathogenesis of preterm birth (Rellán et al., 2008):
- maternal-dependent factors: reproductive factors, illnesses, toxic habits, gynecological factors, stress, having been preterm…,
- fetal factors (congenital anomalies, intrauterine growth restriction, infections, loss of fetal well-being…),
- multiple pregnancy,
- complications specific to the pregnancy: preeclampsia, premature rupture of membranes…
However, in 70% of cases, preterm labor occurs spontaneously making primary prevention difficult, as a consequence of a premature onset of labor (45%) or a premature rupture of membranes (25%). The remaining 30% correspond to medically indicated cases to advance delivery due to maternal or fetal problems (Rellán et al., 2008). It is important to mention the widespread increase in prematurity rates in the last 10–20 years.
This increase can be attributed in our environment to a multitude of factors occurring at the same time, such as advances in perinatal care, improvements in assessment methods, increased maternal age and therefore a higher prevalence of diseases such as diabetes mellitus or arterial hypertension, greater demand and use of assisted reproduction techniques (not only does multiple pregnancy increase risk, but it also increases even if the pregnancy is singleton). The growing number of late preterm infants has influenced this rise in prematurity rates, while the percentage of births at a gestational age equal to or less than 32 weeks has remained unchanged (Rellán et al., 2008).
In summary, the PNB population is very heterogeneous with regard to etiology, clinical presentation, complications and prognosis, requiring multidisciplinary care.

Subscribe
to our
Newsletter
Brain injury in the preterm newborn
Following Dr. Miranda (2006), prematurity per se, together with all the stimuli to which the brain is exposed in the extrauterine environment, affects to a greater or lesser extent the normal brain development of the PNB, which will depend on intrauterine brain development, the age and cause of prematurity, perinatal pathology (episodes of hypoxia, hypotension, hypo-hypercapnia, infections…), the intensive treatment the child requires in the first weeks of life and the type, location and magnitude of possible brain lesions. The brain of an extremely preterm infant at 40 weeks has less complexity in its sulci and gyri, less volume and less white matter maturation than that of a term newborn (Miranda, 2006).
Neurological/neuropsychological complications are common in the PNB, and it is usual for multiple factors to be present at the same time or successively to generate more than one type of lesion (Cerisola et al. 2019).
In the PNB the most frequent CNS pathology will be constituted by: intracranial hemorrhages (VIC), lesions of the white matter ($B) and cerebellar lesions.
Intracranial hemorrhage (ICH)
Among the ICHs that occur in the PNB are included germinal matrix hemorrhage (GMH), intraventricular hemorrhage (IVH) and parenchymal hemorrhages, the latter being the least frequent. Both GMH and IVH can be grouped under the term peri-intraventricular hemorrhage (PV-IVH) and it is the main complication that can lead to brain injury in the PNB.
The most frequent origin of hemorrhages in the PNB’s brain is the germinal matrix (GM), a structure located in the periventricular subependymal region that is highly vascularized. When a GMH occurs, it can rupture the underlying ependyma and penetrate into the ventricles, thus constituting IVH (Ballabh, 2014)
PV-IVH is classified into different grades defined by the presence or absence of hemorrhage in the ventricles, the percentage of intraventricular hemorrhage, and the presence or absence of periventricular hemorrhagic infarction.
- Grade I: the hemorrhage is localized in the subependymal GM,
- Grade II: there is intraventricular blood occupying less than 50% of the ventricle area and without ventricular dilation,
- Grade III: there is intraventricular blood occupying more than 50% of the ventricle area and with ventricular dilation.
- Grade IV: intraventricular and intraparenchymal hemorrhage, corresponding to periventricular venous hemorrhagic infarction.
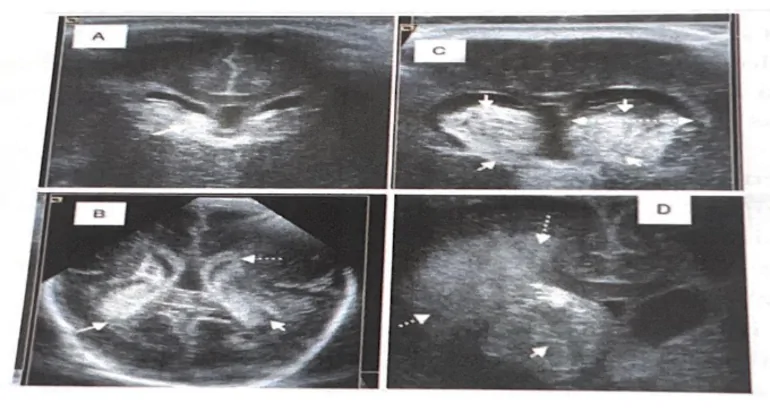
Hemorrhage at this level will cause a loss of its cellular progenitors and, due to the pressure caused by the hemorrhage and the resulting oxidative stress, the lesion of the surrounding WM will be aggravated, contributing to periventricular leukomalacia (PVL) (Cerisola et al., 2019.
GMH occurs in the PNB as a result of multiple factors. According to studies by Ballabh (2014) on its pathogenesis, “it will be the fragility of the blood vessels that prepares the ground and hemodynamic fluctuations, together with a lack or immaturity of autoregulatory mechanisms, that trigger the hemorrhage.” Important risk factors related to hemodynamic fluctuations include situations such as: vaginal delivery, a low APGAR score, severe respiratory distress, pneumothorax, hypoxia and hypercapnia, seizures, patent ductus arteriosus, infections… Platelet and coagulation disorders will act as aggravating factors in this situation (Ballabh, 2014).
Neuropsychological rehabilitation in preterm infants
Babies born before 37 weeks are considered premature. They are at risk of developmental problems, both cognitive and motor. Cognitive development refers to thinking and learning abilities. Motor development refers to the ability to move, crawl or walk.
Therefore, preterm children are more likely to develop some neuropsychological pathology. These pathologies can be more or less severe. Among them learning difficulties, ADHD, auditory, visual or language disorders, dyslexia, ASD or cerebral palsy stand out.
Pediatric neuropsychological rehabilitation is aimed at children who have neurological disorders that affect their functional capacity. The goal is to achieve their maximum autonomy and help them develop their abilities.
Thus, pediatric neuropsychological rehabilitation begins in the first months of life and, in many cases, has a preventive character.
Right Now it is worth asking whether there is scientific evidence of the benefits of this early intervention.
Is early intervention beneficial?
According to a study by Alicia Spittle, Jane Orton and others, early intervention programs for preterm infants have a positive influence on cognitive and motor levels during childhood. In addition, the cognitive benefits persist into preschool age.
On the other hand, no evidence was found of a positive long-term effect in adulthood of these cognitive or motor benefits.
Therefore, the aim of this rehabilitation is to enhance cognitive development by reducing the likelihood of cognitive and motor problems in the short and medium term.
Bibliography
- Abbott, A. (2015). Neuroscience: The brain, interrupted. Nature, 518(7537), 24-26.https://dor.org/10.1038/518024ª
- Abiramalatha, T., Bandyopadhyay, T., Ramaswamy, V. V., Shaik, N. B., Thanigainathan, S., Pullattayil, A. K., & Amboiram, P. (2021). Risk Factors for Periventricular Leukomalacia in Preterm Infants: A Systematic Review, Meta-analysis, and GRADE-Based Assessment of Certainty of Evidence. Pediatric Neurology, 124, 51-71. https://doi.org/10.1016/j.pediatrneurol.2021.08.003
- Ancel, P.-Y., Goffinet, F., EPIPAGE-2 Writing Group, Kuhn, P., Langer, B., Matis, J.. Hernandorena, X., Chabanier, P., Joly-Pedespan, L., Lecomte, B., Vendittelli, F., Dreyfus, M., Guillois, B., Burguet, A., Sagot, P., Sizun, J., Beuchée, A., Rouget, F., Favreau, A., … Kaminski, M. (2015).
- Survival and morbidity of preterm children born at 22 through 34 weeks’ gestation in France in 2011: Results of the EPIPAGE- Conor study. JAMA1693), https://doi.org/10.1001/jamapediatrics.2014.3351
- Anderson, V., Northam, E., & Wrennall, J. (2018). Developmental Neuropsychology: A Clinical Approach. Psychology Press.
- Ballabh, P. (2014). Pathogenesis and prevention of intraventricular hemorrhage. Clinics in Perinatology, 41(1), 47-67. https://doi.org/10.1016/j.clp.2013.09.007
- Baron, I. S. (2018). Neuropsvchological Evaluation of the Child: Domains, Methods, and Case Studies. Oxford University Press.
- Bax, M., Goldstein, M., Rosenbaum, P., Leviton, A., Paneth, N., Dan, B., Jacobsson, B. Damiano, D., & Executive Committee for the Definition of Cerebral Palsy. (2005). Proposed definition and classification of cerebral palsy, April 2005. Developmental Medicine Child Neurology, 478),571-576. https://doi.org/10.1017/s001216220500112x
- Beaino, G., Khoshnood, B., Kaminski, M., Marret, S., Pierrat, V., Vieux, R., mThiriez, G., Matis, J., Picaud, J.-C., Rozé, J.-C., Alberge, C., Larroque, B., Bréart, G., Ancel, P.- Y., & EPIPAGE Study Group. (2011). Predictors of the risk of cognitive deficiency in very preterm infants: The EPIPAGE prospective cohort. Acta Paediatrica (Oslo, Norway: 1992), 100(3), 370-378. https://doi.org/10.1111/j.1651-2227.2010.02064.x
- Beauchamp, M. H., Peterson, R. L., Ris, M. D., ‘Taylor, H. G., & Yeates, K. O. (2022). Pediatric Neuropsychology: Research, Theory, and Practice. Guilford Publications.
- Burstein, O., Zevin, Z., & Geva, R. (2021). Preterm Birth and the Development of Visual Attention During the First 2 Years of Life: A Systematic Review and Meta-analysis. JAMA Network Open 43), e213687.https://doi.org/10.1001/jamanetworkopen.2021.3687
- Cantallops, A. E., & Rovira, T. R. (2015). Neuropsicologia pediátrica. Editorial Sintesis.
- Castro-Caldas, A., Petersson, K. M., Reis, A., Stone-Elander, S., & Ingvar, M. (1998). The illiterate brain. Learning to read and write during childhood influences the functional organization of the adult brain. Brain: A Journal of Neurology, 121 (Pt 6), 1053-1063. https://doi.org/10.1093/brain/121.6.1053
- Cerisola, A., Baltar, F., Ferrán, C., & Turcatti, E. (2019). Mecanismos de lesión cerebral en niños prematuros. Medicina (Buenos Aires), 79, 10-14. Chakraborty, R., Vijay Kumar, M. J., & Clement, J. P. (2021). Critical aspects of neurodevelopment. Neurobiology of Learning and Memory, 180, 107415. https://doi.org/10.1016/j.nlm.2021.107415
- Dennis, M. (1988). Language and the young damaged brain. En Clinical neuropsychology and brain function: Research, measurement, and practice (pp. 89-123). American Psychological Association. https://doi.org/10.1037/10063-003
- Díez-Cirarda, M., Yus, M., Gómez-Ruiz, N., Polidura, C., Gil-Martínez, L., Delgado-Alonso, C., Jorquera, M., Gómez-Pinedo, U., Matias-Guiu, J., Arrazola, J., & Matias-Guiu, J. A. (2022). Multimodal neuroimaging in post- COVID syndrome and Correlation with cognition. Brain, awac384. https://doi.org/10.1093/brain/awac384
- Federación Estatal de Asociaciones de Profesionales de Atención Temprana. (2005). Libro Blanco de la Atención Temprana. Real Patronato sobre Discapacidad.
- Fuentefria, R. do N., Silveira, R. C., & Procianoy, R. S. (2017). Motor development of preterm infants assessed by the Alberta Infant Motor Scale: Systematic review article. Jornal De Pediatría, 934),328-342. https://doi.org/10.1016/j.jped.2017.03.003
- García, P., San Feliciano, L., Benito, F., García, R., Guzmán, J., Salas, S., Fernandez, C., del Prado, N., Ciprián, D., & Figueras, J. (2013). Evolución a los 2 años de edad corregida de una cohorte de recién nacidos con peso inferior o igual a 1.500 g de los hospitales pertenecientes a la red neonatal SEN1500. Anales de Pediatria, 795), 279-287. https://doi.org/10.1016/j.anpedi.2013.03.017
- García Reymundo, M., Hurtado Suazo, J. A., Calvo Aguilar, M. J., Soriano Faura, F. J., Ginovart Galiana, G., Martin Peinador, Y., Jiménez Moya, A., & Demestre Guasch, X. (2019). Recomendaciones de seguimiento del prematuro tardio. Anales de Pediatria, 905), 318.el-318.8. https://doi.org/10.1016/j.anpedi.2019.01.008
- Garrido, A., Alfonso, M., Gómez, M., Niño, G., Patiño, M., & Luque, Y. (2014). Edad motora versus dad corregida en infantes prematuros y con bajo peso al nacer. Revista de Facultad de Medicina, 62, 205-211. https://doi.org/10.15446/revfacmed.v62n2.45376
- GAT. (s. f.). Libro Blanco de la Atención Temprana. Retrieved November 6, 2022, From https://www.observatonodelainfancia.es/ora/esp/documentos_ficha.aspx?id=807
- GERRARD-MORRIS, A., TAYLOR, H. G., YEATES, K. O., WALZ, N. C., STANCIN, T., MINICH, N., & WADE, S. L. (2010). Cognitive development after traumatic brain injury in young children. Journal of the International Neuropsvchological Society:JINS, 161), 157-168. https://doi.org/10.1017/S1355617709991135
- Gerrard-Morris, A., Taylor, H. G., Yeates, K. O., Walz, N. C., Stancin, T., Minich, N., & Wade, S. L. (2010). Cognitive development after traumatic brain injurv in voung children. Journal of the International Neuropsychological Society: JINS, 16(1), 157-168. https://doi.org/10.1017/S1355617709991135
- Gotardo, J. W., Volkmer, N. de F. V., Stangler, G. P., Dornelles, A. D., Bohrer, B. B. de A., & Carvalho, C. G. (2019). Impact of peri-intraventricular haemorrhage and periventricular leukomalacia in the neurodevelopment of preterms: A svstematic review and meta-analvsis. PloS One, 1410), e0223427. https://doi.org/10.1371/journal.pone.0223427
If you liked this article about clinical neuropsychology in prematurity and neurodevelopment, you will surely be interested in these NeuronUP articles:
“This article has been translated. Link to the original article in Spanish:”
Neuropsicología clínica en la prematuridad y neurodesarrollo




 What is frontotemporal dementia and how does it affect?
What is frontotemporal dementia and how does it affect?
Leave a Reply