In this article we address how to enhance cognitive rehabilitation by ethically using the placebo effect grounded in scientific evidence.
Introduction
The placebo effect can significantly influence the outcomes of cognitive stimulation, even in the absence of treatments with active ingredients. Understanding its neurobiological and psychological bases allows neurorehabilitation professionals to design more effective interventions, improving adherence, patient motivation and therapeutic outcomes.
Below we explore what the placebo effect is, how it affects cognition, what the latest scientific evidence says and how professionals such as neuropsychologists, occupational therapists and speech therapists can apply it in their cognitive rehabilitation programs.
What is the placebo effect? Definition and neurobiological mechanisms
The placebo effect is defined as the improvement in health or in the symptoms of a disease resulting from the patient’s belief and expectation of receiving an effective treatment, even though it does not contain active pharmacological ingredients (Benedetti, 2009). In the field of cognitive stimulation, understanding it is key to enhancing the impact of non-pharmacological treatments.
Main neurobiological mechanisms of the placebo effect
- Dopaminergic system and endogenous opioid system: Activation of these neurochemical pathways promotes the release of neurotransmitters such as dopamine and endorphins, which can activate reward circuits, modulate pain perception and improve mood (Benedetti, 2021).
- Classical conditioning and associative learning: The patient’s previous experiences with effective therapies can generate conditioned responses to contextual stimuli, such as the clinical environment or the therapist’s language. This mechanism involves brain structures such as the amygdala, the hippocampus and the anterior cingulate cortex, and depends on dopamine release in the nucleus accumbens (Wager & Atlas, 2015; Colloca & Benedetti, 2005).
- Expectation and conscious processing: belief in the efficacy of the treatment activates regions such as the dorsolateral prefrontal cortex, the thalamus, the anterior insula and the nucleus accumbens, areas involved in attention, emotional regulation and the anticipation of rewards (Wager & Atlas, 2015; Kaptchuk et al., 2010).
Open-label placebo vs. deceptive placebo
An important distinction in placebo research is the difference between the deceptive placebo (deceptive placebo) and the open-label placebo (open-label placebo).
In the deceptive placebo, the patient receives a inactive intervention believing it contains an active ingredient. This modality has shown robust therapeutic effects in various pathologies, due to the activation of positive expectations and neurobiological mechanisms such as the dopaminergic system, the endogenous opioid system or the modulation of pain and anxiety (Benedetti, 2009; Wager & Atlas, 2015).
Unlike the deceptive placebo, the open-label placebo is administered by informing the patient that what they are receiving is a placebo. Recent studies have explored its effects in various conditions, showing that, in some cases, despite that knowledge by users, symptomatic and clinical improvements can be observed (Kaptchuk et al., 2020). This phenomenon represents an innovative and ethically acceptable approach.
The mechanism of the open-label placebo is based on conscious expectation, prior conditioning and the activation of brain networks related to attention, motivation and the anticipation of improvement. In addition, it highlights the power of psychoeducation, the therapeutic alliance and the way the intervention is presented as key factors to enhance the patient’s response.

Subscribe
to our
Newsletter
Recent scientific evidence of the placebo effect in clinical and cognitive contexts
Recent scientific literature has shed light on the clinical relevance of the placebo effect in contexts related to cognitive stimulation, neuropsychiatric disorders and functional rehabilitation.
Although the placebo does not replace active therapies, it can enhance their effects when managed ethically and in a structured way.
1. Placebo effect in post-stroke rehabilitation
A meta-analysis by Jin Y et al. (2021) evaluated the effects of sham repetitive transcranial magnetic stimulation (sham rTMS) in patients with stroke. From 26 clinical studies, a medium-sized placebo effect was found (Hedges’ g ≈ 0.47), with improvements observed in motor and cognitive function that persisted for at least 3 months. This suggests that the therapeutic framework and the patient’s expectations can act as important adjuvants in neurological rehabilitation.
2. Placebo effect in mental disorders such as depression and anxiety
An umbrella review by Huneke NT et al. (2023), which analyzed more than 1,700 randomized clinical trials in psychiatry, showed that the placebo produces significant improvements in various mental disorders such as major depression, generalized anxiety disorders and chronic pain. These results consolidate the therapeutic role of expectations in the treatment of emotional and somatic symptoms.
3. Placebo as an enhancer of psychotherapy
Schienle A and Jurinec N. (2022) demonstrated that the use of open-label placebo as a complement to cognitive behavioral therapy (CBT) for depression significantly increased symptom reduction, compared with CBT alone. The authors attribute these results to the interaction between conscious expectation, the therapeutic alliance and the positive intervention context. This finding supports the hypothesis that conscious positive suggestion can potentiate standard psychological treatments.
4. Placebo in anxiety and neuropathic pain
The meta-analysis by Fernández-López R et al. (2022) analyzed more than 80 studies on placebo in generalized anxiety, finding a medium effect (SMD ≈ 0.45), comparable to some low-dose anxiolytics. Meanwhile, the study by Cragg JJ et al. (2016) showed clinically relevant placebo effects in the treatment of central neuropathic pain, a condition common in neurodegenerative diseases and acquired brain injury.
5. Open-label placebo: mixed results in healthy populations
Hartmann et al. (2023) evaluated the use of open-label placebo for 21 days in healthy adults without neurological or psychiatric diagnoses. Despite generating high adherence and positive perception, no significant improvements were found in memory, attention or processing speed, indicating that the placebo effect is more evident in clinical or vulnerable populations.
How does the placebo effect influence cognitive stimulation?
The placebo effect impacts the patient’s response to cognitive stimulation not only at a neurobiological level, but also through psychosocial factors that modulate therapeutic efficacy (Benedetti, 2009; Wager & Atlas, 2015).
These factors enhance cognitive rehabilitation when integrated into the clinical design and application:
- Positive patient expectations: belief in the treatment’s efficacy activates brain circuits related to motivation and reward anticipation, increasing engagement and performance during cognitive tasks (Kaptchuk et al., 2010; Wager & Atlas, 2015).
- Therapeutic context and environment: a structured, safe and motivating environment reduces anxiety and facilitates sustained attention, optimizing learning and recovery capacity (Benedetti, 2021).
- Strong therapeutic relationship: the therapeutic alliance based on empathy and clear communication promotes greater adherence and a positive perception of progress, key elements for success in neurorehabilitation (Benedetti, 2021; Kaptchuk et al., 2020).
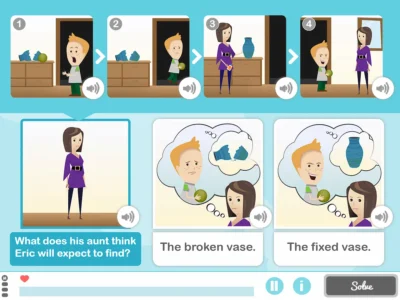
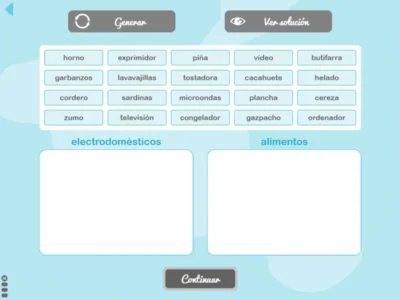
- Emotional and symbolic reinforcement: elements such as positive feedback, gamification and attractive visual materials act as reinforcers that amplify the therapeutic response, enhancing motivation and perceived self-efficacy (Meeuwis et al., 2022; Qin et al., 2020).
Thus, the placebo effect can be considered a mechanism that amplifies the real impact of cognitive stimulation, contributing to better functional outcomes when these factors are properly leveraged in clinical intervention.
Practical recommendations for neurorehabilitation professionals
Neurorehabilitation professionals can ethically and effectively integrate knowledge about the placebo effect into their interventions:
1. Design positive and motivating therapeutic experiences
- Take care of the environment and the presentation of activities: use attractive materials, tidy spaces and technology that facilitates interaction.
- Verbally reinforce each achievement, no matter how small, to build confidence and a sense of progress.
- Incorporate gamification elements and immediate feedback to maintain interest and motivation (Meeuwis et al., 2022).
2. Foster realistic and optimistic expectations
- Explain clearly how and why cognitive stimulation can help, avoiding exaggerated promises or false hopes.
- Involve the patient in understanding their process, emphasizing their active role in improvement (Benedetti, 2021).
- Use positive messages that enhance self-efficacy and perceived control over recovery (Wager & Atlas, 2015).
3. Strengthen the therapeutic alliance
- Listen actively, validate emotions and show constant empathy.
- Maintain clear, honest and consistent communication that generates trust and safety.
- Set shared goals and personalize the treatment according to individual needs and expectations (Kaptchuk et al., 2020).
4. Monitor results with rigor and objectivity
- Combine validated subjective measures, such as the Visual Analogue Scale (VAS), the Patient Global Impression of Change (PGIC) or the Beck Depression Inventory-II (BDI-II), with standardized neuropsychological tests, such as the MoCA, the Trail Making Test, or the RAVLT, to distinguish between real improvements and expectation-driven effects.
- Carry out periodic assessments that allow adjusting the intervention and detecting possible biases related to the placebo effect.
- Record progress to reinforce the perception of advancement, without losing sight of scientific objectivity (Qin et al., 2020).
Conclusion
The placebo effect in cognitive stimulation and mental health is a real neurobiological phenomenon with relevant clinical implications. When understood and managed ethically, it can improve treatment efficacy, increase patient adherence and enhance therapeutic motivation.
For neurorehabilitation professionals, integrating strategies that activate this effect in a natural and transparent way represents an opportunity to maximize clinical benefits without foregoing scientific evidence.
References
- Benedetti, F. (2009). Placebo Effects: Understanding the mechanisms in health and disease. Oxford University Press.
- Benedetti, F. (2011). The Patient’s Brain: The neuroscience behind the doctor-patient relationship (2nd ed.). Oxford University Press.
- Colloca L, Miller FG. The nocebo effect and its relevance for clinical practice. Psychosom Med. 2011 Sep;73(7):598-603. doi: 10.1097/PSY.0b013e3182294a50. Epub 2011 Aug 23. PMID: 21862825; PMCID: PMC3167012.
- Cragg JJ, Warner FM, Finnerup NB, Jensen MP, Mercier C, Richards JS, Wrigley P, Soler D, Kramer JLK. Meta-analysis of placebo responses in central neuropathic pain: impact of subject, study, and pain characteristics. Pain. 2016 Mar;157(3):530-540. doi: 10.1097/j.pain.0000000000000431. PMID: 26588698.
- Enck P, Benedetti F, Schedlowski M. New insights into the placebo and nocebo responses. Neuron. 2008 Jul 31;59(2):195-206. doi: 10.1016/j.neuron.2008.06.030. PMID: 18667148.
- Fernández-López R, Riquelme-Gallego B, Bueno-Cavanillas A, Khan KS. Influence of placebo effect in mental disorders research: A systematic review and meta-analysis. Eur J Clin Invest. 2022 Jul;52(7):e13762. doi: 10.1111/eci.13762. Epub 2022 Feb 27. Erratum in: Eur J Clin Invest. 2022 Oct;52(10):e13854. doi: 10.1111/eci.13854. PMID: 35224726; PMCID: PMC9286474.
- Hartmann H, Forkmann K, Schmidt K, Kleine-Borgmann J, Albers J, Wiech K, Bingel U. Open-label placebo treatment does not enhance cognitive abilities in healthy volunteers. Sci Rep. 2023 Nov 9;13(1):19468. doi: 10.1038/s41598-023-45979-3. PMID: 37945662; PMCID: PMC10636058.
- Huneke NT, Amin J, Baldwin DS, Chamberlain SR, Correll CU, Garner M, Hill CM, Hou R, Howes OD, Sinclair JM, Solmi M, Cortese S. Placebo effects in mental health disorders: protocol for an umbrella review. BMJ Open. 2023 Nov 30;13(11):e073946. doi: 10.1136/bmjopen-2023-073946. PMID: 38035741; PMCID: PMC10689367.
- Jin Y, Pu T, Guo Z, Jiang B, Mu Q. Placebo effect of rTMS on post-stroke motor rehabilitation: a meta-analysis. Acta Neurol Belg. 2021 Aug;121(4):993-999. doi: 10.1007/s13760-020-01460-w. Epub 2020 Aug 8. PMID: 32772334.
- Kaptchuk, T. J., et al. (2010). Placebos without deception: A randomized controlled trial in irritable bowel syndrome. PLoS ONE, 5(12), e15591.
- Schienle A, Jurinec N. Open-label placebos as adjunctive therapy for patients with depression. Contemp Clin Trials Commun. 2022 Jun 16;28:100948. doi: 10.1016/j.conctc.2022.100948. PMID: 35754973; PMCID: PMC9228278.
- Wager, T. D., & Atlas, L. Y. (2015). The neuroscience of placebo effects: Connecting context, learning and health. Nature Reviews Neuroscience, 16(7), 403–418.
Frequently asked questions about the placebo effect
1. What is the placebo effect in cognitive stimulation?
It is the perceived or real improvement in cognitive performance caused by the patient’s positive expectation, without a change in the active treatment.
2. Does the placebo improve cognitive functions?
Yes, especially in motivated patients and in well-designed therapeutic contexts. Its effect is limited in healthy populations.
3. What is an open-label placebo and is it ethical?
Yes. The open-label placebo informs the patient that there is no active ingredient, but it relies on conscious expectation. It has scientific support in multiple studies.
4. Can the placebo effect be measured in neurorehabilitation?
Yes. It is recommended to use objective tests and repeat measurements to distinguish between real improvements and expectation-induced improvements.
5. Should I use the placebo effect as a therapeutic strategy?
Not as a substitute, but as an enhancer. Integrating it ethically can improve treatment efficacy.
If you liked this article about the placebo effect in cognitive stimulation, you will probably be interested in these NeuronUP articles:
“This article has been translated. Link to the original article in Spanish:”
Efecto placebo en estimulación cognitiva: Qué es, evidencia científica y claves clínicas para aplicarlo en neurorrehabilitación





 Cognitive rehabilitation at the University of Navarra Clinic with NeuronUP: an experience of innovation and humanization
Cognitive rehabilitation at the University of Navarra Clinic with NeuronUP: an experience of innovation and humanization
Leave a Reply