The neuropsychologist Ana Isabel Moneo Troncoso, referring to the incomplete infarct and to the capacity offered by the Cognitive Stimulation (CS) technique to promote neuronal plasticity, explains the importance of early neurorehabilitation in cases of Stroke (ACV) for greater recovery.
What is a stroke?
The stroke, ictus or apoplexy, refers to the acute neurological injury that arises due to a pathological alteration in the blood vessels, giving rise to one of the neurological diseases with the highest incidence in recent years and a primary public health problem.
In cases of rupture of a blood vessel it is referred to as what is known as a “hemorrhagic stroke,” corresponding to 15% of cases. When a clot forms causing a decrease in blood flow, it is referred to as an “ischemic stroke,” corresponding to 85% (Zhao et al., 2022).
Stroke is associated with impairment both at the physical and cognitive levels, producing deterioration. Once the damage occurs, the cognitive sequelae affect between 25 and 80% of survivors, leading to alterations in cognitive functioning (Mane, Chouhan and Guan, 2020).
Among the most frequent impairments are difficulties:
- in the attentional domain (selective and divided),
- in the memory domain (storage and retrieval),
- at the executive level (organization and planning)
- mood alterations among others.
For this reason, it is especially important to focus attention on comprehensive rehabilitation, taking the cognitive domain into consideration since the sequelae limit the patient’s autonomy and quality of life (Ardila, Silva and Acosta, 2013).
The role of brain-derived neurotrophic factor in neuronal survival
Once the lesion occurs, selective necrosis (non-physiological cell death due to irreparable or incurable damage, causing putrefaction) is produced that would affect a group of cells within the area, preserving some neuronal cells, glia and microvasculature. After the partial cell death termed “incomplete infarct” the presence of surviving neurons is detected even two days after the damage occurs. Recent advances show the importance of Brain-Derived Neurotrophic Factor (BDNF), the most highly expressed protein in the Central Nervous System, present from 7 to 14 days after the lesion (Jiang et al., 2017).
Brain-Derived Neurotrophic Factor (BDNF)
BDNF is a protein located in neuronal dendrites and axons, involved in neurogenesis or the formation of new neurons, in cell differentiation, in the process of apoptosis or programmed cell death and in neuronal survival. In cases of neurological disorders, it plays essential roles in the reorganization of damage through the activation of different pathways.
As a consequence of the damage, proliferation and a migratory cell stream toward the injured region occur, with changes in the migratory process being linked to the neurotrophic factor (Pisani et al., 2023).
The protective effects of the protein stand out, being involved both in axonal and dendritic growth as well as in synaptic establishment and maintenance, facilitating long-term potentiation (LTP) (which will be explained later). For this reason, it is worth highlighting the neuroprotective and brain regeneration role of BDNF in cases of damage (Simko, Kent and Rektorova, 2022).
The protein’s localization is found mainly in cortical, amygdaloid, cerebellar and hippocampal areas, the latter region being linked to learning and memory. Activation of intracellular processes has been evidenced following BDNF activation, promoting the underlying processes of learning and memory.
Given the key role of the protein in counteracting damage, early rehabilitation is essential for improving cognitive functioning and therefore greater recovery (Pisani et al., 2023).
Post-stroke rehabilitation through cognitive stimulation
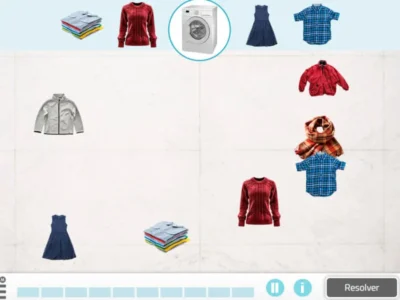
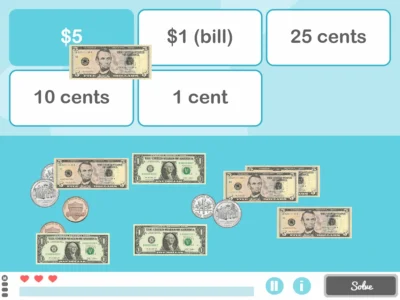
Cognitive Stimulation (CS) is one of the rehabilitation techniques with the most evidence in stroke as shown by the scientific literature. It refers to the set of techniques and strategies aimed at optimizing the effectiveness of the functioning of different cognitive capacities and functions (perception, attention, reasoning, abstraction, memory, language, orientation processes and praxias). All of this is achieved through a series of specific situations and activities that are structured in what are called “cognitive training programs” (Villalba and Espert, 2014).
The neurobiological bases that determine the effectiveness of the intervention are based both on neuroplasticity and on cognitive reserve, among others. The term neuroplasticity refers to the modifiable nature of human behavior since the brain has a great capacity to adapt to new situations and restore balance after damage. Because the nervous system is extremely plastic, changes can occur both at the structural and functional levels and therefore, an improvement in synaptic plasticity favoring recovery (Castillo, Fernández and Chamorro, 2020).

Subscribe
to our
Newsletter
Synaptic plasticity
The term synaptic plasticity refers to the connection between adjacent neurons allowing the passage of information. Neural circuits are routes of communication exchange that are modified through learning and practice. After acquiring new knowledge, through synaptic communication, repeated practice over time improves communication and therefore the connections become strengthened (which is called LTP).
Cognitive reserve
The term cognitive reserve refers to the brain’s ability to tolerate brain injuries in the absence of cognitive and behavioral symptoms. Stimulation over the years through the acquisition of knowledge, physical activities and social contact increases this reserve, which results in a delay in the clinical expression of cognitive deficits (Kwakkel, Kollen and Lindeman, 2004).
Transcranial Direct Current Stimulation (tDCS)
Recent advances in the field of rehabilitation show combined therapies of CS and other techniques, such as Transcranial Direct Current Stimulation (tDCS) for cognitive improvement since both techniques offer benefits when applied separately.
tDCS is a non-invasive and painless brain neuromodulation technique aimed at modulating regional cortical excitability or inhibition instantly, using two electrodes placed on the scalp (Conde-Antón et al., 2020).
The neural changes are linked to the modulation of activity in neurotransmitters (dopamine, serotonin, glutamate and acetylcholine among others) and alterations in the neurotrophic factor. After the application of tDCS, BDNF is modulated which favors neuronal growth and connections, improving damage recovery (Madeiros et al., 2012).

Subscribe
to our
Newsletter
Conclusion
Given the noticeable increase in stroke cases in recent years, knowledge about the benefits of early neurorehabilitation in cases of stroke is essential. Not only are the sequelae minimized by the damage, but it also offers an improvement in the patient’s cognitive and functional ability. All of this will lead to a positive impact on perceived quality of life, greater autonomy and an improvement in mood which reduces social isolation. Therefore, there will be an improvement in family dynamics benefiting patients, as well as relatives and/or caregivers.
Bibliography
- Ardilla, W., Silva, F. y Acosta, M.R. (2013). Neuropsychological profile in patients with ischemic stroke of the left middle cerebral artery. Acta Neurología Colombia 29 (1), 36-43.
- Castillo, G., Fernández, B. y Chamorro, D. (2020). Neuroplasticity: Exercises to delay the effects of Alzheimer’s Disease through Cognitive Stimulation. Revista Investigación científica tecnológica 4 (2), 115-122.
- Conde-Antón, A., Hernando-Garijo, I., Jiménez-del-Barrio, S., Mingo-Gómez, M.T., Medrano-de-la-Fuente, R. y Ceballos-Latia, L. (2020). Effects of transcranial direct current stimulation and transcranial magnetic stimulation in patients with fibromyalgia. Systematic review. Neurología, 38 (2023), 427-439.
- Jiang, M.Q., Zhao, Y.Y., Cao, W., Wei, Z.Z., Gu, X., Wei, L. y Yu, S.P. (2017). Long-term survival and regeneration of neuronal and vasculature cells inside the core region after ischemic stroke in adult mice. Brain Pathol 27(4), 480-498.
- Kwakkel, G., Kollen, B. y Lindeman, E. (2004). Understanding the pattern of functional recovery after stroke: facts and theories. Restor Neurol Neurosci 22 (3-5), 281-99.
- Mane, R., Chouhan. T. y Guan, C. (2020). BCI for stroke rehabilitation: motor and beyond. J Neural Eng. 17 (4), 1-21.
- Medeiros, L., de Souza, I., Vidor, LP., de Souza, A., Deitos, A., Volz, MS., Fregni, F., Caumo, W. y Torres, IL. (2012). Neurobiological effects of transcranial direct current stimulation: a review. Front Psychiatry, 3 (110), 1-11.
- Pisani, A., Paciello, F., Del Vecchio, V., Malesci, R., De Corso, E., Cantone, E., y Fetoni, A. R. (2023). The Role of BDNF as a Biomarker in Cognitive and Sensory Neurodegeneration. Journal of personalized medicine, 13(4), 652.
- Skimo, P., Kent, J., Rektorova, I. (2022). In non-invasive brain stimulation effective for cognitive enhancement in Alzheimer`s disease? An updated metaanalysis. Clinical Neurophysiology 144, 23-40.
- Villalba, S. Y Espert, R. (2014). Cognitive stimulation: A neuropsychological review. Therapeía 6 73-93.
- Zhao, Y. Zhang, X., Chen, X. y Wei, Y. (2022). Neuronal injuries in cerebral infarction and ischemic stroke: From mechanisms to treatment (Review). International Journal of Molecular Medicine 49, 1-9.
If you liked this article about the importance of early neurorehabilitation in cases of stroke, you will surely also be interested in:
“This article has been translated. Link to the original article in Spanish:”
Neuronas supervivientes. La importancia de la neurorrehabilitación precoz en casos de accidente cerebrovascular




 Clinical Neuropsychology in Pediatric Epilepsy Neurosurgery
Clinical Neuropsychology in Pediatric Epilepsy Neurosurgery
Leave a Reply