Neuropsychologist Javier Tomás addresses the concept of scaffolding in neurorehabilitation. How the collaboration between patient and therapist in neurorehabilitation processes allows gains that an automatic, closed program cannot achieve.
My uncle (who is a bricklayer) says that a poor mix in the components of cement or concrete can ruin any structure that is perfect on paper. In neurorehabilitation we sometimes experience the same.
Scaffolding
Why do many professionals not understand that collaboration between the patient and the therapist allows gains that an automatic, closed program cannot achieve? Open computer systems, even at the risk of experiencing non-generalization in experimentation, have clinical power. What is it? That they allow your patient to understand their abilities in a real way. That they are meaningful. That they focus on real tasks.
Effectiveness and Efficacy
It is the same difference between the terms effectiveness and efficacy. It is good to remember that Cicerone (who is hardly lacking in rigor) uses the term effectiveness to define treatments in neuropsychological rehabilitation in the Cochrane reviews. That is, in neurorehabilitation we want things that are effective (with clinical potency and a solid background theoretical basis based on evidence), rather than efficacious (with experimental rigor, without that implying a strong background theoretical basis). Which allows an additional question to be posed: are medical and pharmacological experimental models extrapolable to research in neuropsychological rehabilitation? This is a question that would make for a good debate, but let us focus on the gains of something clinically relevant. To illustrate this topic a little, we are going to analyze a term called scaffolding in rehabilitation. The term has several meanings, so here we go:
Scaffolding as a process
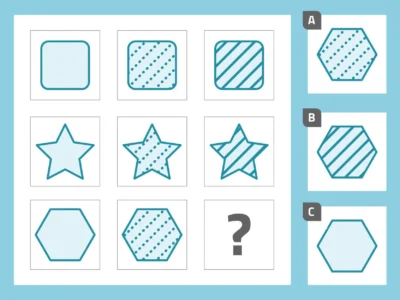
“Method of task analysis in which the therapist controls aspects of the task that are beyond the patient’s range of activity, allowing them to concentrate on aspects that are within their competence” (Wood, Brunner Ross, 1976, p. 90). It provides maximum support to the patient but without being an errorless learning method. Responsibility in a task is transferred little by little, and allows the patient to know their real performance. It is based on a very basic principle: If the patient improves in task execution, in the next phase of the task they are given more control; if they fail, the therapist takes greater control.
All this allows the patient to gain awareness of their strengths and weaknesses, and to anticipate errors. It differs from successive approximations to tasks, and from grading the difficulty of a task in that the scaffolding method does not focus exclusively on simplified versions of the target-task (a difficult or advanced level activity), graded by the therapist: it focuses on a collaboration in which both subjects (therapist and patient) are active, not passive. Of course a videogame is interactive. But a therapist/family member analyzing how you use a videogame, giving you feedback… besides being interactive is clinically more effective. It allows identifying the targets of treatment.
Scaffolding as a guide or instruction in a sequenced task
Part of the ideas of Luria and Vigotsky (Zone of Proximal Development), who proposed a parental method of verbal guidance for the execution of tasks in children. It is a verbal guide during the execution of the task that serves as support to the subject. External verbal aids are a help for the patient, an added capability that allows the patient to perform the task better than if done without help. It is aimed at: initiation of behavior, generalization, problem solving, planning, sequencing, monitoring… Basically the therapist functions as an external central executive to the patient. Useful in the early stages of rehabilitation and in the learning of new behaviors that can be sequenced. One of the requirements is that verbal comprehension, memory and motor response to verbal commands must be preserved. We have already begun to propose a system of visual instructions.
With ecological tasks, it has been shown that patients make fewer errors and need fewer attempts to learn (Curran, 2004). But it takes more time (and this goes against the much-vaunted time-cost-effectiveness). My question: isn’t it worth taking longer to rehabilitate a patient, but to rehabilitate them better? By the way, these techniques can also be taught to caregivers and have been shown to improve performance in ADLs (a good idea for the guide for relatives that we are proposing in a LinkedIn group to which you are all invited). Sohlberg also refers to this type of instruction in some reviews.

Subscribe
to our
Newsletter
Scaffolding as a specific graphic technique
A new alternative we want to develop is a graphic scaffolding of concepts (a behavior diagram). In this scaffolding the patient would have to develop an action scheme in which they graphically break down behaviors, and can make notes on those behaviors. For example, a route model for buying bread could receive a scaffolding treatment, with specific behaviors and decisions. It is a visual model in which there is a graphic representation of the control processes to carry out an ADL.
Scaffolding as a neural process
Proposed, among others, by Denise C. Park (2009). Park’s neuroimaging research reaches the following conclusion: as we grow older, when we face a task with a high demand we activate more areas of the frontal lobe (which manage cognitive resources that are located in other posterior regions of the brain), producing a greater scaffolding of neuronal structures. This maturation results in an increase in cognitive capacities as long as scaffolding is approached as a global process (diet, exercise, cognitive coping style…). These studies serve to propose active aging, in which the loss of reaction time or processing speed is compensated by other functions.

What do all these meanings have in common?
That they are personalized. They are meaningful. They are flexible. And they are effective. And they require therapist–patient collaboration. And maybe they are mistaken about one thing. That we are not only supervisors of the construction. We are also bricklayers (workers) of the brain, we help build neural connections. We are part of the human factor in neurorehabilitation.
Comments and constructive criticism are welcome.
Best regards!
PS1: The LinkedIn group in which we are discussing these issues together with other professionals is called “La familia como parte del proceso rehabilitador”.
PS2: This is an excerpt of a paragraph in English that I found which explains the difference between efficacy and effectiveness: “(…) there are different standards of proof for establishing the efficacy of an intervention as opposed to its effectiveness. Efficacy refers to whether the intervention can be successful when it is properly implemented under controlled conditions, whereas effectiveness refers to whether the intervention typically is successful in actual clinical practice”.
Another meaning:
Effectiveness VS Efficacy: Effective treatment provides positive results in a usual or routine care condition that may or may not be controlled for research purposes but may be controlled in the sense of specific activities are undertaken to increase the likelihood of positive results. Effectiveness studies use real-world clinicians and clients, and clients who have multiple diagnoses or needs. In contrast, Efficacious treatment provides positive results in a controlled experimental research trial. A study that shows a treatment approach to be “efficacious” means that the study produced good outcomes, which were identified in advance, in a controlled experimental trial, often in highly constrained conditions. Translating efficacious practices to routine practice settings to produce effective results is one of the more challenging issues of evidence-based practice.
If you liked this post about scaffolding, you might be interested in these NeuronUP articles.
“This article has been translated. Link to the original article in Spanish:”
El andamiaje: un buen concepto en la neurorrehabilitación




 Intensive therapies in neurorehabilitation: applicable only to motor functions?
Intensive therapies in neurorehabilitation: applicable only to motor functions?
Leave a Reply