Irma Otero Vázquez, a general health psychologist and therapist, explores Lewy body disease, attributing great importance to its symptomatology and its differences with Parkinson-associated dementia and Alzheimer’s disease.
The increase in the population’s life expectancy has caused the incidence and prevalence of neurodegenerative diseases to soar. Dementia due to Lewy bodies underlies a large part of this problem, so knowing and treating it will be essential to reduce its socioeconomic and personal costs.
What are Lewy bodies?
Lewy bodies are abnormal accumulations of the protein alpha-synuclein that form in the nervous system at cortical and subcortical levels. It has been shown that abnormalities in this protein cause neuronal dysfunction or, in some cases, neuronal death. This leads to a significant reduction in dopamine, a cholinergic pathology and dysfunctions in other neurotransmitters, giving rise to a specific symptomatology. Therefore, disorders that present this etiology are called alpha-synucleinopathies (Prasad et al., 2023).
The neurodegenerative diseases/dementias can be classified based on various criteria and one of them is molecular pathology (Kovacs, 2017), in which alpha-synucleinopathies and, therefore, Lewy bodies would be grouped.
Lewy body disease
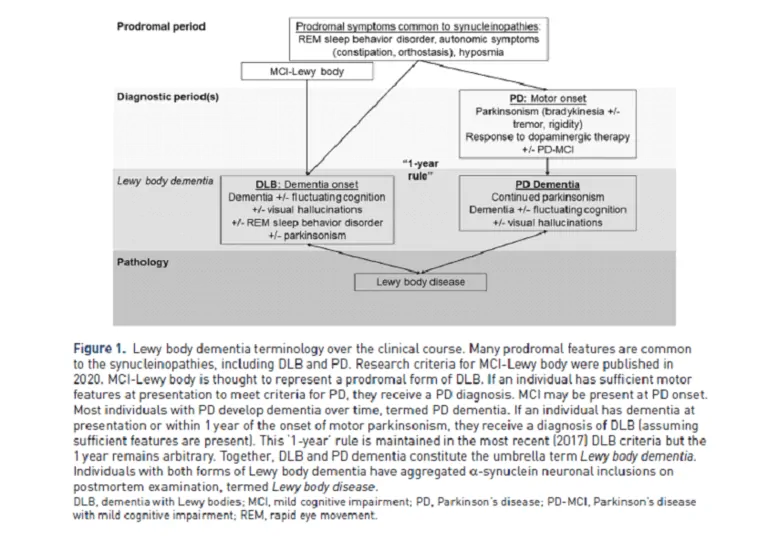
The concept of Lewy body disease has recently been proposed to encompass a group of alpha-synucleinopathies that present these formations due to the clinical and pathological overlap between disorders (Menšíková et al., 2022). In this way, we include the following clinicopathological entities:
- Parkinson’s disease.
- Dementia with Lewy bodies (which encompasses Parkinson’s disease dementia and dementia with Lewy bodies).
- Multiple System Atrophy.
Therefore, terminology will be very important when referring to one
pathology or another.
It should be noted that motor, cognitive, behavioral and psychological presentations differ between entities, so this heterogeneity in their symptomatology and course is something we must keep very much in mind. The basis behind this is still limited but certain studies suggest that the concomitant presence of beta-amyloid and tau pathologies, characteristic of Alzheimer’s disease, could influence these differences (Coughlin et al,. 2020).
Dementia with Lewy bodies
Dementia with Lewy bodies is the second most frequent cause of neurodegenerative disorder, after Alzheimer’s disease, in people over 75 years of age. Despite this, the prevalence reported by different studies is variable. This may indicate its underdiagnosis since it is sometimes incorrectly classified as Alzheimer-type dementia or as Parkinson’s disease with mild cognitive impairment due to its symptomatic similarity (Milán-Tomás, Fernández-Matarrubia and Rodríguez-Oroz, 2021).
Its etiology is unknown, but an interaction between genetic and environmental factors is proposed (Bellas-Lamas, 2012). As for whether Lewy body dementia is hereditary, most cases are sporadic. However, some autosomal dominant inheritance cases with mutations in certain genes have been reported (Walker et al., 2015).
This disorder usually begins between the ages of 70 and 80, its onset tends to be insidious, and it is associated with a faster functional decline than Alzheimer’s disease, with a fluctuating and progressive course (Bellas-Lamas et al., 2012).
Symptomatology
There are a number of core features in the presentation of dementia with Lewy bodies that encompass Parkinson’s disease dementia and dementia with Lewy bodies.
Parkinsonism
This symptom results from the loss of dopaminergic neurons in the nigrostriatal pathways and the presence of Lewy bodies. Bradykinesia and rigidity are the most common signs (>85%). Parkinsonism is usually symmetric and signs of extrapyramidal dysfunction as well as myoclonus are often observed. All of this increases the risk of swallowing problems or falls, and there is a poor response to levodopa/carbidopa medication unlike what occurs in Parkinson’s disease (Prasad et al., 2023).
REM sleep behavior disorder
This is a parasomnia in which the typical muscle atonia of REM sleep is deficient. It is present in 76% of patients and is characterized by actions, vocalizations and movements that reflect what is happening in their dreams. It usually appears years before other symptoms and may be accompanied by confused awakenings, daytime sleepiness, insomnia… (Prasad et al., 2023).
Cognitive fluctuations
These fluctuations are similar to what happens during an episode of delirium and refer to marked differences in levels of cognition, attention and arousal, sometimes causing daytime sleepiness or alterations in the thought process. Behavioral changes, incomprehensible speech, altered consciousness or deterioration of visuospatial skills may also occur (Gomperts, 2016 y Milán-Tomás et al 2021).
Hallucinations
The most common are visual hallucinations, which occur in 80% of patients. These are typically of great complexity and emotionally neutral, often taking the form of animals or people with much detail. People are usually aware of them and report them to other family members. Sometimes a sense of presence or of someone walking nearby is also described. Auditory hallucinations are less frequent and are usually verbal (Prasad et al., 2023).
Impaired regulation of the autonomic nervous system
The prevalence of this type of symptomatology is 90%, the most common being: orthostatic hypotension, urinary incontinence, hyposmia, constipation, erectile dysfunction, gastroparesis or seborrhea (Prasad et al., 2023; Bellas-Lamas et al., 2012).
Hypersensitivity to neuroleptics
The loss of dopaminergic neurons in these patients is partly responsible for hypersensitivity to antipsychotics. As a consequence of taking them, parkinsonism tends to worsen and the risk of mortality increases due to neuroleptic malignant syndrome. Certain manifestations of these people can be assessed in emergency settings as psychotic symptoms, administering this class of drugs with important consequences for their health (Gomperts, 2016).

Subscribe
to our
Newsletter
Neuropsychological profile of Lewy body dementia
Once the core characteristics of dementia with Lewy bodies have been discussed, we will focus particularly on the neuropsychological profile of dementia with Lewy bodies (DLB) since it differs somewhat from that associated with Parkinson’s disease.
Patients with this pathology exhibit both cortical and subcortical alterations (Yubero et al., 2011), particularly affecting the cognitive functions outlined below.
On the one hand, visuoconstructive deficits are observed from prodromal stages of the disease, in which errors are identified when reproducing complex figures such as the Rey figure. Some authors indicate that these alterations may be due more to the existence of visuoperceptual and praxis problems, so assessment should be detailed in this respect (Kempt et al., 2017). In addition, deficits in visuospatial tasks can be observed such as, for example, tasks of discriminating shapes and sizes and in the visual organization of objects (Yubero, 211). Likewise, attentional and executive function failures are exhibited, especially related to distractibility, inhibition, task initiation, attentional shifting and working memory. As for mnemonic function, deficits are mild and relatively stable at first (Subirana et al., 2011), although errors in visual recognition should be noted, while verbal memory seems to be more preserved. However, these difficulties may be due to visual or attentional disturbances. In addition, in this area failures in information retrieval were also observed (Kempt et al., 2017). Finally, in the language area, the greatest alterations were found in relation to verbal fluency (Yubero et al., 2011).
Regarding neuropsychiatric manifestations, symptoms of anxiety, depression and apathy are the most common and tend to present from the start and persist during the development of the disease (Donaghy et al., 2018 y Prasad et al., 2023).
Differences between dementia with Lewy bodies and Parkinson-associated dementia
DLB and Parkinson-associated dementia share around 85% of symptoms, making them difficult entities to differentiate. The key criterion to discern between one disorder and another is temporal (Martini 2020), as McKeith et al. established in 2017 indicating that if cognitive symptoms began before or within the year prior to the presentation of parkinsonism, the diagnosis of dementia with Lewy bodies is established (Armstrong, 2021). In addition, extrapyramidal symptoms are usually more evident in Parkinson-associated dementia.
Cognitively there are differentiating symptoms such as visuospatial and visuoconstructive functions and visual and verbal memory, which tend to be more impaired in DLB, and visual hallucinations and delusions are also more common in it (Milán-Tomás et al., 2021). Another differentiating factor is the levels of amyloid accumulation in the brain parenchyma, more common in DLB (Prasad et al., 2023).
Differences between dementia with Lewy bodies and Alzheimer’s disease (AD)
DLB and AD in their initial phase share certain similarities that make their correct diagnosis difficult, such as failures in episodic memory, present in both pathologies (Yubero, 2011). However, this is not entirely correct since the errors exhibited in AD are related to storage and encoding processes, unlike those of DLB, whose problem lies in retrieval processes (Ciofane et al., 2019). For its part, in the visuospatial domain the decline is sharper and faster in DLB (Milán-Tomás et al., 2021), as well as in attentional deficits, with fluctuations not present in AD, and in executive and visuoconstructive function. The latter is disproportionately affected in relation to the rest of the DLB alterations (Yubero, 2011).
Treatment of dementia with Lewy bodies
Currently there are no effective therapies that can modify the course of Lewy body dementias. Therefore, intervention is aimed at treating the most prominent symptoms in order to alleviate their impact on the quality of life of both the person and their environment (Milán-Tomás et al., 2021).
Starting with pharmacological treatments, we will pay attention to those that worsen the person’s clinical picture such as benzodiazepines and opioids, among others. Besides, for each symptom there are different pharmacological options: for cognitive symptoms cholinesterase inhibitors are recommended, donepezil and rivastigmine, while for sleep disorders melatonin is commonly used (Armstrong, 2021).
Regarding non-pharmacological treatments, which have positioned themselves as an appropriate therapeutic option to treat this class of pathologies, we can talk about physical therapy (which could be beneficial in managing extrapyramidal signs), occupational therapy, speech therapy and swallowing assessments (recommended to improve dysphagia, prevent falls and improve functionality), cognitive rehabilitation (for its impact on quality of life, satisfaction and mood) and environmental modifications or music therapy (for improving behavioral symptoms) (Guidi et al., 2023 and Armstrong, 2023).
In summary, the therapeutic approach in this type of pathology must be carried out from a multidisciplinary perspective in order to address this wide range of symptomatology.
Conclusions
Dementia with Lewy bodies is a much broader construct than was thought a few years ago and the fine lines that differentiate one pathology from another can be very complicated to discern. That is why, as professionals, we must be extremely careful in our assessments, so that we can pick up those key signs and symptoms that will guide us to a more accurate diagnosis. The importance of this does not lie in simply having achieved a good pathological classification, but in that it will be very useful when proposing an appropriate treatment that truly improves the quality of life and functionality of the users and caregivers.
Bibliography
- Armstrong, M. J. (2021). Advances in dementia with Lewy bodies. Therapeutic Advances in Neurological Disorders, 14, 17562864211057666.
- Bellas Lamas, P., Rodríguez Regal, A., & Cebrián Pérez, E. (2012). Demencia por cuerpos de Lewy. Rev. neurol.(Ed. impr.), s67-s74.
- Ciafone, J., Little, B., Thomas, A. J., & Gallagher, P. (2020). The neuropsychological profile of mild cognitive impairment in Lewy body dementias. Journal of the International Neuropsychological Society, 26(2), 210-225.
- Coughlin, D. G., Hurtig, H. I., & Irwin, D. J. (2020). Pathological influences on clinical heterogeneity in Lewy body diseases. Movement Disorders, 35(1), 5-19.
- Donaghy, P. C., Taylor, J. P., T O’Brien, J., Barnett, N., Olsen, K., Colloby, S. J., … & Thomas, A. J. (2018). Neuropsychiatric symptoms and cognitive profile in mild cognitive impairment with Lewy bodies. Psychological medicine, 48(14), 2384-2390.
- Gomperts, S. N. (2016). Lewy body dementias: dementia with Lewy bodies and Parkinson disease dementia. Continuum: Lifelong Learning in Neurology, 22(2), 435-463.
- Guidi, L., Evangelisti, S., Siniscalco, A., Lodi, R., Tonon, C., & Mitolo, M. (2023). Non-pharmacological treatments in Lewy body disease: a systematic review. Dementia and Geriatric Cognitive Disorders, 52(1), 16-31.
- Kemp, J., Philippi, N., Phillipps, C., Demuynck, C., Albasser, T., Martin-Hunyadi, C., … & Blanc, F. (2017). Cognitive profile in prodromal dementia with Lewy bodies. Alzheimer’s research & therapy, 9, 1-10.
- Kovacs, G. G. (2018). Concepts and classification of neurodegenerative diseases. In Handbook of clinical neurology (Vol. 145, pp. 301-307). Elsevier.
- McKeith, I. G., Boeve, B. F., Dickson, D. W., Halliday, G., Taylor, J. P., Weintraub, D., … & Kosaka, K. (2017). Diagnosis and management of dementia with Lewy bodies: Fourth consensus report of the DLB Consortium. Neurology, 89(1), 88-100.
- Menšíková, K., Matěj, R., Colosimo, C., Rosales, R., Tučková, L., Ehrmann, J., … & Kaňovský, P. (2022). Lewy body disease or diseases with Lewy bodies?. npj Parkinson’s Disease, 8(1), 3.
- Milán-Tomás, Á., Fernández-Matarrubia, M., & Rodríguez-Oroz, M. C. (2021). Lewy body dementias: a coin with two sides?. Behavioral Sciences, 11(7), 94.
- Prasad, S., Katta, M. R., Abhishek, S., Sridhar, R., Valisekka, S. S., Hameed, M., … y Walia, N. (2023). Recent advances in Lewy body dementia: A comprehensive review. Disease-a-Month, 69(5), 101441.
- Risacher, S. L., & Saykin, A. J. (2019). Neuroimaging in aging and neurologic diseases. Handbook of clinical neurology, 167, 191-227.
- Subirana, J., Basté, M. C., Gómez, N. C., Pérez, R. C., & Signo, S. (2011). Demencias y enfermedad de Alzheimer. In Rehabilitación neuropsicológica: intervención y práctica clínica (pp. 289-317). Elsevier.
- Walker, Z., Possin, K. L., Boeve, B. F., & Aarsland, D. (2015). Non-Alzheimer’s dementia 2: Lewy body dementias. Lancet (London, England), 386(10004), 1683.
- Yubero, R. (2011). Características neuropsicológicas y aproximación diagnóstica a la demencia Parkinson ya la demencia por cuerpos de Lewy. Revista Española de Geriatría y Gerontología, 46, 12-18.
If you liked this article about Lewy bodies, you will surely be interested in these NeuronUP articles:
“This article has been translated. Link to the original article in Spanish:”
Enfermedad de cuerpos de Lewy




 Episodic Memory Game for Adults: Remember the Names (Audio)
Episodic Memory Game for Adults: Remember the Names (Audio)