Neuropsychologist Estefanía Lesser explains the benefits of cognitive stimulation for older adults with depression, as well as the most effective strategies.
Introduction
In the first part of this article we analyzed how depression in older adults affects cognitive functions and why cognitive stimulation represents a key strategy for addressing it. Below, we explore the specific benefits of this intervention, practical strategies and the fundamental role of the therapeutic team.
Benefits of cognitive stimulation for older adults with depression
The cognitive stimulation produces positive effects across multiple dimensions of functioning in older adults with depression, especially when carried out systematically and within an interdisciplinary approach. The benefits are not limited solely to the cognitive domain, but also extend to emotional and social well-being.
Cognitive benefits of cognitive stimulation for older adults with depression
- Improvement in memory: Improvements are observed in working memory, verbal memory and recognition, functions especially sensitive to aging and depression (Jean et al., 2010; Gates et al., 2011).
- Increased attention and concentration: Regular participation in mental exercises stimulates sustained attention and selective attention, which facilitates performance of daily activities (Kinsella et al., 2009).
- Stimulation of language and verbal fluency: Activities such as reading, guided conversation and naming exercises help preserve language and communication skills (Crespo et al., 2012).
- Strengthening of reasoning and cognitive flexibility: Problem-solving and training of executive functions increase adaptability and decision-making capacity (Reijnders et al., 2013).
Emotional and social benefits of cognitive stimulation for older adults with depression
- Reduction of social isolation: Participating in group or interactive sessions stimulates interpersonal contact, strengthening the sense of belonging and motivation (Bahar-Fuchs et al., 2013).
- Increase in self-esteem and sense of achievement: Overcoming cognitive challenges gives the older adult a more positive perception of themselves, which is fundamental to counteracting the hopelessness associated with depression (Cummings et al., 2019).
Recommended frequency and duration of cognitive stimulation programs for older adults with depression
The benefits of cognitive stimulation are more evident when applied with structure, continuity and personalization. The literature suggests:
- Optimal frequency: 2 to 3 times per week.
- Session duration: between 45 and 60 minutes.
- Total program duration: a minimum of 12 weeks to observe significant effects, although long-term interventions are recommended to sustain results (Olazarán et al., 2010; Sitzer et al., 2006).
Programs should be adapted to the level of impairment and emotional state of the patient, and integrated with other psychotherapeutic or pharmacological interventions when required.

Subscribe
to our
Newsletter
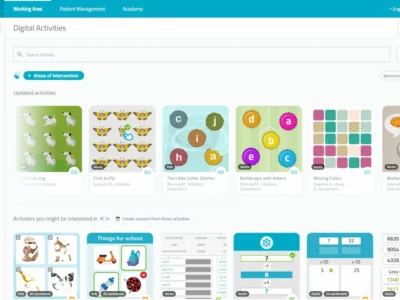
Effective cognitive stimulation strategies for older adults with depression
Cognitive stimulation strategies should be personalized, meaningful and adapted to the functional level and emotional state of the older adult. Below, widely used techniques are described, along with their cognitive benefits and emotional impact:
- Structured mental games (crosswords, Sudokus, word searches, memory-type games):
- Cognitive benefits: They improve sustained attention, working memory and logical reasoning.
- Emotional impact: They foster motivation, reduce boredom and reinforce the sense of competence and achievement (Jean et al., 2010; Reijnders et al., 2013).
- Time-orientation and spatial exercises (identifying date, season, location, context):
- Cognitive benefits: They reinforce situational awareness and reduce disorientation.
- Emotional impact: They increase the sense of control and reduce anxiety in new or confusing contexts (Bahar-Fuchs et al., 2013).
- Use of external aids and visual reminders (agendas, calendars, notes, alarms, reminder boards):
- Cognitive benefits: They promote functional autonomy and prospective memory.
- Emotional impact: They reduce frustration and enhance confidence in daily life (Crespo et al., 2012).
- Reminiscence therapies (use of photographs, old music, personal objects, life stories):
- Cognitive benefits: They stimulate autobiographical memory and verbal recall.
- Emotional impact: They promote personal identity, strengthen emotional bonds and reduce isolation (Woods et al., 2018).
- Guided reading and functional writing (summaries, free writing, reading aloud, diaries):
- Cognitive benefits: They reinforce language, reading comprehension and written expression.
- Emotional impact: They promote creativity, self-expression and reflective thinking (Gates et al., 2011).
These activities should be carried out in non-threatening contexts, valuing the patient’s interests to facilitate adherence and avoid feelings of failure.
Complementary support: mindfulness
Although it is not strictly a cognitive stimulation strategy, the practice of mindfulness can play a relevant role as a complementary technique. It has been shown that mindfulness improves emotional self-regulation, sustained attention and stress management ability, which can favor the older adult’s willingness to participate in cognitive activities (Lenze et al., 2014; Geiger et al., 2016).
- Emotional impact: Reduction of mild depressive symptoms, improved mood and increased perceived well-being.
- Suggested application: brief sessions of guided meditation, mindful breathing or body-scan exercises integrated into the routine.
It is essential that activities are meaningful and adapted to the patient’s interests to avoid frustrations and increase adherence.
Multidisciplinary approach in cognitive stimulation for older adults with depression
The therapeutic approach for older adults with depression and cognitive impairments should be carried out from a multidisciplinary approach, in which various professionals act in a coordinated manner to intervene in the multiple dimensions of the patient’s functioning.
Below are the specific roles of each member of the team:
- Neuropsychologists: They are responsible for the comprehensive assessment of the cognitive functions using standardized tests. They develop an individualized cognitive profile that allows designing stimulation plans adjusted to the detected deficits. In addition, they apply specific cognitive rehabilitation techniques and monitor neuropsychological changes (Ardila & Ostrosky-Solís, 2018).
- Clinical psychologists: They focus on the management of emotional, behavioral and motivational aspects of the older adult with depression. They use psychotherapeutic interventions, mainly from the cognitive-behavioral approach, to reduce affective symptoms and strengthen adherence to stimulation programs (Areán et al., 2010). Unlike the neuropsychologist, their work is not centered on cognitive performance but on overall psychological well-being.
- Psychiatrists: They participate in the diagnostic and pharmacological evaluation of the patient. In cases of major depression or psychiatric comorbidities, they are key to establishing and adjusting psychopharmacological treatments that facilitate the patient’s participation in the other interventions (Jeste et al., 1999).
- Occupational therapists: Intervene in activities of daily living (ADLs), seeking to preserve or recover functional autonomy. They apply structured activities that integrate cognitive stimulation with practical skills, reinforcing the connection between cognitive training and everyday functionality (Padilla, 2011).
- Speech-language therapists: Assess and treat speech, communication and swallowing disorders, functions that directly impact the quality of life and social interaction of the older adult. Good communication strengthens self-esteem, participation and motivation to get involved in cognitive activities (Cummings, 2019).
- Physiotherapists: Improve mobility, balance and overall physical condition. This not only prevents falls and favors independence, but also contributes to executive and emotional functioning, since physical exercise is associated with improvements in attention, processing speed and mood (Forbes et al., 2015).
The follow-up of the process is carried out through periodic interdisciplinary team meetings, where progress is evaluated, therapeutic goals are adjusted and cognitive stimulation strategies are redesigned according to the patient’s clinical, emotional and functional status.
Conclusion
Depression in older adults is a common condition, often underdiagnosed, that affects both emotional state and cognitive functioning. Alterations in attention, memory and executive functions not only reduce quality of life, but can also mimic more severe impairment, as occurs in depressive pseudodementia. This reinforces the need for precise clinical and neuropsychological assessments.
In this context, cognitive stimulation for older adults is consolidated as an effective therapeutic tool to prevent, treat and compensate the cognitive and functional effects of depression in late life. Its usefulness goes beyond the neuropsychological field, positively impacting self-esteem, sense of purpose, motivation and the social relationships of the older person.
Implementing these cognitive stimulation strategies for older adults with depression requires a multidisciplinary approach, in which each professional neuropsychologists, clinical psychologists, occupational therapists, speech-language therapists, physiotherapists and psychiatrists– contributes a specific and complementary perspective.
Finally, considering older adults as active participants in their cognitive stimulation process is key to promoting healthier, more autonomous and dignified aging. Integrating these interventions into routine clinical care represents an ethical and social commitment to a population that is often made invisible in its cognitive and emotional needs.
If you didn’t get to read the first part of this article about cognitive stimulation in older adults with depression, you can consult it from here.
Bibliografía
- Areán, P. A., Raue, P., Mackin, R. S., Kanellopoulos, D., McCulloch, C., & Alexopoulos, G. S. (2010). Problem-solving therapy and supportive therapy in older adults with major depression and executive dysfunction. American Journal of Psychiatry, 167(11), 1391–1398. https://doi.org/10.1176/appi.ajp.2010.09091327
- Ardila, A., & Ostrosky-Solís, F. (2018). Neuropsicología clínica: Diagnóstico y tratamiento de los trastornos cognitivos. Editorial Manual Moderno.
- Bahar-Fuchs, A., Clare, L., & Woods, B. (2013). Cognitive training and cognitive rehabilitation for mild to moderate Alzheimer’s disease and vascular dementia. Cochrane Database of Systematic Reviews, 2013(6), CD003260. https://doi.org/10.1002/14651858.CD003260.pub2
- Crespo, M., López, J., & Rivas, M. T. (2012). Intervenciones para la mejora del funcionamiento cognitivo en personas mayores. Revista Española de Geriatría y Gerontología, 47(4), 173–181. https://doi.org/10.1016/j.regg.2012.03.005
- Cummings, J. L., Lyketsos, C. G., & Sweet, R. A. (2019). Cognitive and behavioral aspects of aging: A clinical guide. Oxford University Press.
- Forbes, D., Forbes, S. C., Blake, C. M., Thiessen, E. J., & Forbes, S. (2015). Exercise programs for people with dementia. Cochrane Database of Systematic Reviews, 2015(4), CD006489. https://doi.org/10.1002/14651858.CD006489.pub3
- Gates, N., Sachdev, P. S., Singh, M. A. F., & Valenzuela, M. (2011). Cognitive and memory training in adults at risk of dementia: A systematic review. BMC Geriatrics, 11, 55. https://doi.org/10.1186/1471-2318-11-55
- Geiger, P. J., Boggero, I. A., Brake, C. A., Caldera, C. A., & Segerstrom, S. C. (2016). Mindfulness-based interventions for older adults: A review of the effects on physical and emotional well-being. Mindfulness, 7(2), 296–307. https://doi.org/10.1007/s12671-015-0444-1
- Jean, L., Bergeron, M.-È., Thivierge, S., & Simard, M. (2010). Cognitive intervention programs for individuals with mild cognitive impairment: Systematic review of the literature. The American Journal of Geriatric Psychiatry, 18(4), 281–296. https://doi.org/10.1097/JGP.0b013e3181c37ce9
- Jeste, D. V., Alexopoulos, G. S., Bartels, S. J., et al. (1999). Consensus statement on the upcoming crisis in geriatric mental health: Research agenda for the next two decades. Archives of General Psychiatry, 56(9), 848–853. https://doi.org/10.1001/archpsyc.56.9.848
- Lenze, E. J., Hickman, S., Hershey, T., Wendleton, L., Ly, K., Dixon, D., … & Wetherell, J. L. (2014). Mindfulness-based stress reduction for older adults with worry symptoms and co-occurring cognitive dysfunction. International Journal of Geriatric Psychiatry, 29(10), 991–1000. https://doi.org/10.1002/gps.4096
- Padilla, R. (2011). Effectiveness of interventions designed to modify the activity demands of the occupations of self-care and leisure for people with Alzheimer’s disease and related dementias. American Journal of Occupational Therapy, 65(5), 523–531. https://doi.org/10.5014/ajot.2011.002618
- Reijnders, J., van Heugten, C., & van Boxtel, M. (2013). Cognitive interventions in healthy older adults and people with mild cognitive impairment: A systematic review. Ageing Research Reviews, 12(1), 263–275. https://doi.org/10.1016/j.arr.2012.07.003
- Sitzer, D. I., Twamley, E. W., & Jeste, D. V. (2006). Cognitive training in Alzheimer’s disease: A meta-analysis of the literature. Acta Psychiatrica Scandinavica, 114(2), 75–90. https://doi.org/10.1111/j.1600-0447.2006.00789.x
- Woods, B., O’Philbin, L., Farrell, E. M., Spector, A. E., & Orrell, M. (2018). Reminiscence therapy for dementia. Cochrane Database of Systematic Reviews, (3), CD001120. https://doi.org/10.1002/14651858.CD001120.pub3
Frequently asked questions about the placebo effect
1. What types of cognitive stimulation activities are effective for older adults with depression?
Activities such as crosswords, orientation exercises, reminiscence, guided reading and functional writing, always adapted to the patient’s profile.
2. How many times per week should cognitive stimulation be applied in older adults?
It is recommended to carry out 45-60 minute sessions, 2 to 3 times per week, for at least 12 weeks.
3. What emotional benefits does cognitive stimulation have for older adults?
It improves self-esteem, sense of achievement, reduces isolation and strengthens social and family ties.
4. Can cognitive stimulation be combined with mindfulness or meditation?
Yes. Mindfulness complements the intervention by improving emotional self-regulation and the willingness to participate in activities.
5. Which professionals should coordinate a cognitive stimulation program for older adults with depression?
Neuropsychologists, occupational therapists, clinical psychologists, speech-language therapists, physiotherapists and psychiatrists, working together with caregivers.
If you liked this article about practical strategies for cognitive stimulation for older adults with depression, you will likely be interested in these NeuronUP articles:
“This article has been translated. Link to the original article in Spanish:”
Estrategias prácticas de estimulación cognitiva para adultos mayores con depresión




 Depression in Older Adults: cognitive impact and a stimulation-based approach
Depression in Older Adults: cognitive impact and a stimulation-based approach
Leave a Reply