Ana Isabel Moneo Troncoso, neuropsychologist, presents in this article the role of the ischemic penumbra, neuroimaging techniques, neuroplasticity and neuropsychological rehabilitation in post-stroke recovery.
Introducción
Cerebrovascular disease is one of the frequent reasons for urgent neurological care, posing a major public health problem. One of the most noted findings is the verification that neuronal function can be recovered and survive after a period of hypoxia. Notably, the brain tissue potentially recoverable after injury offers a therapeutic window (a period during which treatment can be most effective). Thanks to technological advances in recent years, significant improvements have been observed in the development of rehabilitation therapies for ischemic injury.
Cerebrovascular disease
Cerebrovascular disease (CVD), also known as “stroke”, refers to the cerebral circulatory disorder that causes a transient or permanent alteration of the function of one or more parts of the brain. Given the nature of the injury, they are differentiated as ischemic or hemorrhagic:
- A hemorrhagic stroke is due to the rupture of a cerebral blood vessel with blood leakage (extravasation) outside the vascular bed,
- whereas an ischemic stroke (85% of cases) is due to a lack of blood supply to a specific area of the brain parenchyma caused by an embolus (blood clot) (Ustrell-Roig y Serena-Leal, 2007).
Given the early evolution in the first hours, two ischemic cerebrovascular events are distinguished:
- the transient ischemic attack (neurological deficit that recovers within the first 24 hours),
- and cerebral infarction (permanent lesion of the brain parenchyma) ischemia of duration sufficient to produce tissue necrosis (De Celis Ruiz et al., 2023).
Cerebrovascular disease is considered a highly prevalent and potentially fatal emergency, representing the second leading cause of death and the leading cause of disability as reported by the World Health Organization (WHO), which constitutes a major public health problem of first order.
After an acute injury there are several windows during which early therapeutic interventions can modify the course of the cerebral infarction and achieve neuronal reactivation:
- Between 6 and 8 hours, intervention to restore blood flow to the affected area (reperfusion);
- between 24 hours and 17 days relates to neuronal survival within the ischemic penumbra;
- finally, a sustained therapeutic focus up to three months is associated with neurofunctional recovery (Sánchez-Chávez, 1999).

Subscribe
to our
Newsletter
Ischemic penumbra
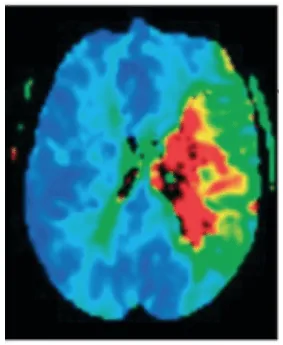
The ischemic penumbra refers to the peripheral brain tissue with functional impairment but potentially recoverable if cerebral ischemia is reversed, considered a potentially viable area thanks to advances in neurorehabilitation. After the ischemic event, the penumbral zone can persist for hours due to the blood supply from collateral arteries, so the presence of a penumbra implies the possibility of cell salvage and an improvement in clinical outcome (Ismael, 2009).
Neuroimaging techniques, such as cranial magnetic resonance imaging, allow confirmation and localization of the lesion’s topography, proving highly useful in the management of the pathology. In the acute phase, the infarcted tissue can be determined thanks to diffusion sequences, as well as the quantification of tissue extent by perfusion sequences (Ustrell-Roig y Serena Leal, 2007).
The positive discrepancy between the volume of the infarct and the volume of the penumbra (mismatch) is used as a predictor of good treatment response (a positive mismatch indicates that there is a large penumbra compared to the infarcted area, which suggests that there is still potentially salvageable brain tissue). Therefore, it is of great relevance to have neuroimaging techniques that allow delineation of the infarct core and the penumbra zone to predict the patient’s prognosis and use it when making therapeutic decisions to select patients who may benefit from reperfusion treatments beyond traditional time windows (García et al., 2022) (figure 1).
Consequently, it is crucial in post stroke rehabilitation to implement both pharmacological and non-pharmacological interventions that ensure the neuroplasticity of brain tissue.
Neuroplasticity
Neuroplasticity, understood from a connectionist perspective, is the capacity of the nervous system for modification and regeneration, allowing nervous tissue to undergo changes of reorganization or adaptation in response to a physiological state with or without alteration. Thanks to brain neuroimaging techniques, it has been possible to determine brain functioning, demonstrating the phenomenon of plasticity, limited not only to childhood and adolescence but throughout adult life (Castillo et al., 2020).
The brain has a great capacity to adapt to circumstances such as brain injury (post-lesion plasticity) compensating damage through reorganization and the creation of new undamaged neuronal connections, making it a highly dynamic and plastic structure (Maurie-Fernández et al., 2010).
Between the initial stages of the ischemic event and the following 3-6 months, a series of processes have been described that demonstrate the operation of plasticity after damage:
- First, there is increased functional activity in the somatosensory system contralateral to the lesion and an identification of cortical regions connected a the affected area.
- Second, strengthening may occur in the structure of the ipsilateral corticospinal pathway to the lesion assuming a compensatory role.
- Finally, the functional connection between the cerebral hemispheres and the sensorimotor cortex network on both sides of the brain is reestablished (Marín-Medina et al., 2023).
The phenomenon of plasticity allows the brain to reconnect and reassign functions to unaffected regions. This compensatory mechanism underpins the neurobiological bases of recovery interventions, such as cognitive stimulation (CS). This compensatory mechanism is crucial, significantly contributing to the rehabilitation and recovery process (Castillo et al., 2020).
Neuropsychological rehabilitation
Neuropsychological rehabilitation, understood as an interactive process, refers to the therapeutic intervention techniques aimed at reducing cognitive, behavioral and emotional deficits after injury, promoting social integration and the patient’s well-being through a therapeutic team. Notable intervention methods include cognitive stimulation, family intervention, behavior modification and professional or vocational readaptation (Murie-Fernández et al., 2010).
In neuropsychological rehabilitation two approaches stand out, restoration and compensation of function.
- The first refers to direct intervention on the altered functions with the aim of achieving partial or total recovery through rehabilitation and repetitive exercises.
- The second refers to learning new strategies to use preserved cognitive abilities when performing tasks that previously required the altered function (CDINC, 2019).
The mechanisms involved in recovery are related to the size, location of the damage, the affected circuit region and the degree of network connectivity. It is noteworthy that, in the case of a moderate lesion with significant network connectivity impairment, treatment based on retraining the function is highly effective (Marín-Medina et al., 2023).
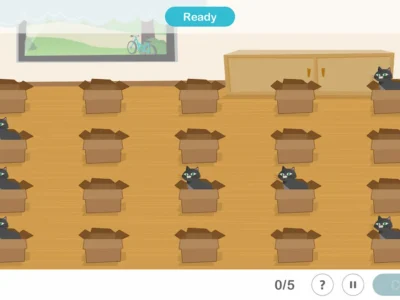
Cognitive stimulation aims at the optimization of cognitive capacities in order to improve cognitive functioning, through training programs based on specific activities. Perception, attention, reasoning, language and memory, among others, are neuropsychological processes that can be improved through cognitive stimulation. However, the affective, social, behavioral and family spheres are also taken into account, resulting in a holistic intervention for the person (Villalba y Espert, 2014).
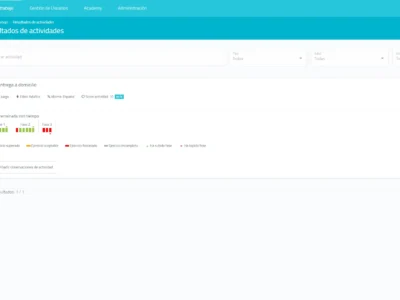
Thanks to significant advances in technology, tools and computer-based cognitive training programs have been developed that allow effective rehabilitation. Among the main advantages offered by information and communication technologies (ICT) in rehabilitation are:
- personalization of treatments according to the specific needs of each patient;
- the provision of immediate feedback after application which promotes patient motivation;
- monitoring of performance in each task;
- as well as a dynamic character of the activities (Fernández et al., 2020).
For all these reasons, ICT represent a milestone in the field of rehabilitation markedly improving the quality of life of ischemic patients, so the synergy between technology and rehabilitation is undeniably a significant advance.
Conclusions
The implementation of new technologies in the rehabilitation of cerebrovascular disease leads to an optimization of therapeutic processes and an improvement of outcomes, facilitating the personalization of interventions. The start of rehabilitation, its duration and intensity are a series of fundamental factors that influence the patient’s functional recovery.
It is of utmost importance that both health authorities and healthcare professionals prioritize care for this pathology, being a crucial factor for the improvement of the healthcare system.
Prioritizing prevention, early diagnosis and prompt, individualized intervention reduces the burden on the health service by promoting comprehensive and effective care. Early attention to cerebrovascular disease should be considered a strategy essential for the well-being of the population.
Bibliografía
- Castillo, G., Fernández, B. and Chamorro, D. (2020). Neuroplasticity: Exercises to delay the effects of the Enfermedad de Alzheimer through Cognitive Stimulation. Revista Investigación científica tecnológica 4(2), 115-122.
- Centro de Diagnóstico e Intervención neurocognitiva (CDINC). (21 de marzo de 2019). What is Neuropsychological Rehabilitation? CDINC. https://cdincbarcelona.com/es/que-es-la-rehabilitacion-neuropsicologica/#:~:text=Seg%C3%BAn%20Organizaci%C3%B3n%20Mundial%20de%20la,adap taci%C3%B3n%20f%C3%ADsica%2C%20psicol%C3%B3gica%20y%20social.
- De Celis Ruiz, E., Masjuan, J., Tejedor, E. D. and De Donlebún, J. R. P. (2023). Ischemic stroke. Cerebral infarction and transient ischemic attack. Medicine-Programa de Formación Médica Continuada Acreditado, 13 (70), 4083-4094.
- Fernández, E., Fernández, and Crespo, M. (2020). Integration of information and communication technologies in neuropsychological intervention. Revista Cubana de Información en Ciencias de la Salud, 31(2).
- García, M. G., Bea, M. P., Saiz, A. A., Fontaneda, V. D. and Leon, E. C. (2022). Update of the stroke code in emergency departments. Radiología, 65(31), 3-10.
- Ismael, M. G. (2009). Contribution of neurospect to the evaluation of the ischemic stroke: ischemic penumbra. Rev. Méd. Clín.Condes, 20(3), 276-281.
- Marín-Medina, D. S., Arenas-Vargas, P. A., Arias-Botero, J. C., Gómez-Vásquez, M., Jaramillo-López, M. F. & Gaspar-Toro, J. M. (2023). New approaches to recovery after stroke. Neurological Sciences, 45(1), 55-63.
- Murie-Fernández, M., Irimia, P., Martínez-Vila, E., John Meyer, M., and Teasell, R. (2010). Neurorehabilitation after stroke. Neurología, 25(3), 189–196.
- Ustrell-Roig, X. y Serena-Leal, J. (2007). Stroke. Diagnosis and treatment of cerebrovascular diseases. Revista Española de Cardiología, 60(7), 753-769.
If you liked this blog post about ischemic penumbra: neurorehabilitation after cerebrovascular disease, you will likely be interested in these NeuronUP articles:
“This article has been translated. Link to the original article in Spanish:”
Penumbra isquémica: Neurorrehabilitación tras la enfermedad cerebrovascular


 Current Trends in the Treatment of Neurodegenerative Diseases
Current Trends in the Treatment of Neurodegenerative Diseases
Leave a Reply