This article presents a clinical summary of post–COVID-19 attentional alterations analyzed in the study “Insights into attention and memory difficulties in post-COVID syndrome using standardized neuropsychological tests and experimental cognitive tasks”.
Introduction
This article is inspired by and based on the study published by Arbula et al. (2024) in Scientific Reports, titled “Insights into attention and memory difficulties in post-COVID syndrome using standardized neuropsychological tests and experimental cognitive tasks”. The study provides a rigorous and innovative framework for the assessment of attentional and memory disorders observed in patients who have recovered from SARS-CoV-2 infection. Based on their conclusions, we offer a clinical synthesis of the post–COVID-19 attentional alterations, integrating classical and experimental assessment methods, as well as adapted therapeutic proposals.
What is post–COVID-19 brain fog and why does it affect attention?
Clinical manifestations of brain fog
Brain fog is not a formal diagnostic entity, but it has become a functional label to describe a constellation of subjective symptoms: difficulty concentrating, frequent forgetfulness, slow thinking, cognitive fatigue, and problems maintaining attention during prolonged or complex tasks.
In clinical contexts, these symptoms resemble those observed in disorders such as myalgic encephalomyelitis, fibromyalgia, or post-concussion syndrome.
Incidence of brain fog in patients recovered from COVID-19
Epidemiological studies indicate that up to 20% of patients who have had COVID-19 show some form of measurable cognitive impairment, with attentional functions being the most commonly affected. In particular, people who were not hospitalized but report subjective cognitive alterations often show sustained difficulties on neuropsychological tests sensitive to attentional control.
Assessment of attention in post–COVID-19 patients
Approach to attention from traditional neuropsychology
Attention has been historically assessed using tests such as the Trail Making Test (TMT), the Stroop Test, the PASAT, or the Symbol Digit Modalities Test. These tools allow detection of alterations in sustained attention, divided attention, and inhibitory control.
In recent studies with post–COVID-19 patients, decreased performance was observed on these tests, even in individuals without prior history of cognitive impairment. This suggests a direct impact of SARS-CoV-2 or its inflammatory consequences on neural circuits involved in attention and frontal executive functions.
Experimental cognitive tasks: a new window
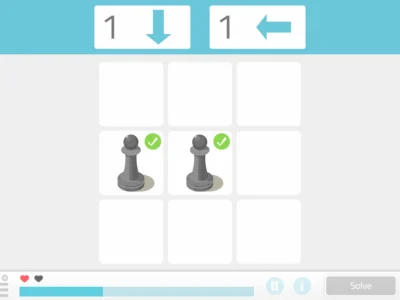
Beyond classical tests, experimental tasks have been developed to more precisely explore specific functions.
For example:
- Flanker task: measures the ability to resolve interference.
- Visual Arrays: evaluates visuospatial selective attention.
- Antisaccade task: explores visual inhibitory control.
These tasks, originally used in research with healthy young adults, have been adapted for clinical populations, allowing detection of subtle deficits that might go unnoticed in conventional batteries.
Main findings about attention post COVID-19
Results from recent studies
A study conducted by Arbula and colleagues (2024) showed that post–COVID-19 patients exhibited significantly lower performance on controlled attention tasks, especially on the Flanker task and Visual Arrays.
- On the Flanker task, patients showed greater difficulty ignoring irrelevant stimuli, indicating impairment in selective attention.
- On Visual Arrays, there was a reduced capacity to retain and manipulate visual information, affecting visuospatial attention.
At the neuropsychological level, alterations were also detected on the Stroop Test and TMT-B, which are sensitive to cognitive interference and mental flexibility, respectively.
Clinical relevance
These results underscore that attention is one of the domains most vulnerable after a COVID-19 infection. This impairment can manifest as:
- Difficulty following complex conversations.
- Problems completing work or academic tasks.
- A feeling of “not being able to think clearly.”
These limitations have a significant impact on quality of life, functional autonomy, and sociolaboral reintegration of the patient.
Influence of emotional state on attention
Anxiety and depression as moderating factors
Post–COVID-19 patients evaluated also showed elevated levels of anxiety (STAI) and depression (BDI), which could act as a confounding or amplifying factor of cognitive symptoms. The literature indicates that affective symptoms can exacerbate subjective complaints, even in the absence of an objective deficit.
Could this be a functional cognitive disorder?
One hypothesis proposed is that in some cases post–COVID-19 attentional dysfunction could be part of a broader picture of functional cognitive disorder, characterized by inconsistent and disproportionate symptoms relative to neuropsychological findings. However, this does not discount the real experience of patients, but rather points to a biopsychosocial model in which emotional and cognitive factors interact.

Subscribe
to our
Newsletter
Clinical recommendations
Multidimensional assessment
Since attentional difficulties can have multiple origins (neurobiological, emotional, functional), an assessment that integrates the following is recommended:
- Standardized neuropsychological tests.
- Specific cognitive tasks.
- Questionnaires of subjective cognitive complaints.
- Evaluation of emotional state (anxiety, depression, posttraumatic stress).
- Meetings with family members.
Personalized intervention
Depending on the patient profile, different therapeutic approaches may be considered:
- Computerized cognitive training: to improve attention sustained attention and inhibitory control.
- Individualized neuropsychological rehabilitation: with compensatory strategies.
- Cognitive-behavioral therapy: aimed at managing anxiety and restructuring dysfunctional beliefs about cognitive performance.
- Group psychoeducational interventions: including information about attentional functioning and techniques of mental hygiene.
Limitations and future research directions
Despite advances, gaps remain in understanding the mechanisms underlying post–COVID-19 attentional deficits:
- It would be important to consider pre–COVID-19 cognitive performance, as this would provide more information about the decline in cognitive functions. If there are tests and results, take them into account.
- It is crucial to investigate the role of systemic inflammation and neurovascular dysfunction as possible mediators of attentional deterioration.
- The study of the implicated neural networks using techniques such as functional MRI or ASL can provide relevant data on structural or functional involvement.
Clinical conclusions about brain fog and attention after COVID-19
Attention is one of the domains most sensitive to post–COVID-19 sequelae. The integration of traditional and experimental methods has allowed identification of subtle deficits that can have a large functional impact. Recognizing, assessing, and treating these problems should be a clinical priority, given their effect on autonomy, work performance, and patients’ mental health.
A multidisciplinary approach that considers both neurocognitive and psychoaffective aspects will be key to providing effective support to people affected by “brain fog” after COVID-19.
Bibliography
- Arbula, S. et al. (2024). Insights into attention and memory difficulties in post-COVID syndrome using standardized neuropsychological tests and experimental cognitive tasks. Scientific Reports, 14(4405). https://doi.org/10.1038/s41598-024-54613-9
- Asadi-Pooya, A. A. et al. (2022). Long COVID syndrome-associated brain fog. J. Med. Virol., 94, 979–984.
- Bhome, R. et al. (2022). Metacognition in functional cognitive disorder. Brain Commun., 4, 1–11.
- Draheim, C. et al. (2021). A toolbox approach to improving the measurement of attention control. J. Exp. Psychol. Gen., 150, 242–275.
- Gouraud, C. et al. (2021). Psychological distress and cognitive complaints after COVID-19. Front. Psychiatry, 12, 1–7.
- Teodoro, T. et al. (2023). Functional neurological disorder in long COVID: A systematic review. Eur. J. Neurol., 30, 1505–1514.
- Velichkovsky, B. B. et al. (2023). Attention and memory after COVID-19. Acta Psychol., 233, 103838.
Frequently asked questions about attention post COVID-19
1. Why is attention affected after COVID-19?
Numerous studies have shown that COVID-19 can cause alterations in the neural circuits responsible for attention, especially in frontoparietal networks. Systemic inflammation, endothelial dysfunction, and changes in brain oxygenation could be involved in this attentional dysfunction, even in patients with mild disease symptoms.
2. What are the most frequent symptoms of an attentional deficit post COVID-19?
Patients usually report difficulties with:
- Concentrating during prolonged tasks.
- Maintaining attention in the presence of multiple stimuli.
- Remembering recent instructions.
- Reading or working without getting easily distracted.
These symptoms significantly impact work, academic, and social functioning.
3. How is attention clinically assessed in post–COVID-19 patients?
Attention can be assessed using:
- Traditional neuropsychological tests, such as the Stroop Test or the Trail Making Test.
- Specific experimental tasks, such as the Flanker task or Visual Arrays.
- Subjective questionnaires, which allow assessment of the patient’s perception of their attention in daily life.
A multidimensional approach improves diagnostic accuracy and allows for designing personalized interventions.
4. Is it possible to recover attention affected by COVID-19?
Yes. Attention is a cognitive function that can be trained and rehabilitated. There are cognitive stimulation programs, both in-person and digital, that have shown efficacy in improving sustained, selective, and divided attention. In addition, addressing emotional factors such as anxiety or depression is fundamental to achieving comprehensive recovery of attention.
5. What strategies can improve attention in daily life?
Some useful strategies to improve attention include:
- Reducing environmental distractions (noise, multitasking).
- Establishing structured routines.
- Using visual or technological reminders.
- Breaking complex tasks into smaller steps.
- Practicing mindfulness techniques, which help train focused attention.
6. What is the difference between an attention problem and a subjective complaint without objective basis?
In some cases, patients may experience a perceived decline in attention without alterations on objective tests. This discrepancy may be due to anxiety, fatigue, or a functional cognitive disorder. However, the complaint should be taken seriously and evaluated by a professional to rule out real attentional deficits.
7. Can attention post COVID-19 be affected long term?
Yes. Although in many cases symptoms are transient, there is a subgroup of patients who continue to experience attention problems for several months or even more than a year after infection. These cases require clinical follow-up, periodic evaluation, and long-term intervention strategies.
If you liked this article about post–COVID-19 brain fog and the clinical assessment of attentional impairment, you will likely be interested in these NeuronUP articles:
“This article has been translated. Link to the original article in Spanish:”
Niebla mental post COVID-19: Evaluación clínica del deterioro atencional





 How the Lescer Center has optimized its therapeutic interventions with NeuronUP
How the Lescer Center has optimized its therapeutic interventions with NeuronUP
Leave a Reply