The psycho-oncologist specialized in pediatrics and child and adolescent psychology, Begoña Acosta, explains in this article the neuropsychological sequelae of childhood cancer, on the occasion of Childhood Cancer Awareness Month which is observed in September.
According to the World Health Organization, cancer, when it appears, does not discriminate in terms of age or the part of the body affected. However, and despite this, did you know that survival from childhood cancer in developed countries is over 80% of diagnosed cases? On the other hand, the reality is that this increase in survival has revealed the neuropsychological sequelae of childhood cancer, among others, in 70% of children and adolescents who are cured. Do you know which types of cancer are most common at this stage and how treatments can influence the appearance of these neuropsychological sequelae of childhood cancer? What are the most common neuropsychological sequelae of childhood cancer and how can they be detected?
Most common types of cancer
Cancer in childhood is considered a rare disease and even so, 400,000 new cases of cancer are diagnosed worldwide each year in those under 18. In Spain, according to the National Registry of Childhood Tumors Observatory of the Spanish Association Against Cancer, 1,006 children aged 0-14 are diagnosed each year, with the most commonly diagnosed types of cancer being the following:
- 30% leukemia,
- 22% central nervous system tumors,
- 20% brain tumors,
- 13% lymphomas.
Diagnosis of the neuropsychological sequelae of childhood cancer
When a child or adolescent receives the diagnosis of cancer in this vital stage it represents a great emotional impact both for the child and for their family.
From that moment they will have to face long hospital stays, medical tests, possible neuropsychological sequelae of cancer and live with the physical and emotional pain that all this entails.
Today, much research is conducted on survivors of childhood cancer and in this line, numerous studies reveal that this population is more prone to develop depression or anxiety in the future, especially if they go on to suffer chronic sequelae resulting from treatments.
The sequelae of cancer in childhood and adolescence are already known as late effects, mainly because they appear or become more evident after treatment. There is something like a critical period in which these sequelae may become evident and research places it from the fourth or fifth year after treatment.
However, it is worth mentioning that known sequelae can also appear at earlier stages, such as the acute stage, which takes place during treatment, and the subacute stage, which is from one to six months after the end of treatment.
Detection of the neuropsychological sequelae of childhood cancer
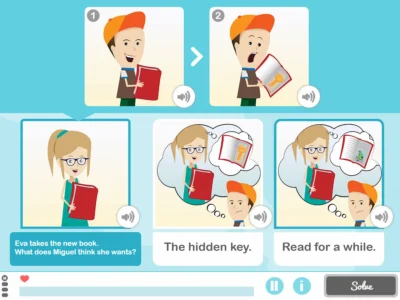
In case of doubt, a specialist in neuropsychology could carry out a neuropsychological assessment and thus the child’s cognitive functions could be studied with the aim of distinguishing those that are preserved and those in which they may present some neurodevelopmental difficulty.
The purpose is to create a personalized cognitive stimulation program that allows the child to develop the cognitive abilities whose development may have been halted during treatments and to rehabilitate the functions that had been previously acquired before treatments and that are currently altered as a consequence of them.
In these cases work is usually carried out in coordination with the school and the family since they are part of the child’s everyday environment.
The neuropsychological intervention will have as its ultimate goal the improvement in quality of life in the face of the neuropsychological sequelae of childhood cancer and the progression in the child’s vital areas that may have been compromised.

Treatments for the neuropsychological sequelae of childhood cancer
The best known and most used treatments for pediatric cancer are chemotherapy, radiotherapy and surgery. All of these share the objective of eliminating malignant cells.
Chemotherapy
It is the most culturally well-known treatment for cancer and its objective is to eradicate cancerous cells, although it can also damage some healthy cells giving rise to some of the known side effects. Some may be transient and others may persist long term despite the end of treatment. This will depend on certain factors mentioned later.
Radiotherapy
This treatment uses high-energy rays to eradicate cancer cells as locally as possible, trying to minimize damage to healthy cells. However, with this treatment the area affected and the age at which it is administered must be taken into account, since the younger the age, the greater the impact both in terms of neuropsychological sequelae of childhood cancer and neuroendocrine effects.
Irradiation in children under three years old is an exceptional practice, normally being delayed until five years of age because of the impact it could have, especially in children irradiated for brain and central nervous system tumors. If damage were to occur later it would tend to be more global than focal, since we are dealing with a developing brain.
Surgery
The possible neuropsychological sequelae of childhood cancer resulting from surgery will largely depend on the type of intervention performed, the person’s health status at the time of surgery and the tumor’s location, among other variables. Surgery often plays an important role in the treatment of pediatric cancer, being considered the first option whenever tumor size allows and/or it is possible.
Modulators of the neuropsychological sequelae of childhood cancer
As mentioned above, the physical and cognitive impact of these treatments will depend on several factors that are considered modulators of the possible appearance of the neuropsychological sequelae of childhood cancer.
In detecting these neuropsychological sequelae of childhood cancer the following should be taken into account:
- The type of cancer, location, the type of treatment, the dose used and the area where it is being administered;
- the age of the child or adolescent when they are diagnosed and when treatments are administered;
- what the child’s state of health was before being diagnosed, even how their health is at the time they are about to begin prescribed treatments or surgery;
- what the genetic and family history related to cancer is. Although it is known that only 5-10% of diagnoses originate from genetic mutations, this factor could influence the other factors mentioned.
These factors intervene in the appearance of the neuropsychological sequelae of childhood cancer and can also give rise to other late effects such as academic and social relationship difficulties, psychiatric diagnoses that compromise personality and mood, as well as neurocognitive dysfunctions.
The neuropsychological sequelae of childhood cancer
According to the research by Bernabeu et al. (2003), there is impairment of neurocognitive functions in children and adolescent survivors of childhood cancer who have been exposed to radiotherapy, chemotherapy and surgery.
Notable is white matter injury, both in leukemias and in brain tumors, and this is due both to the impact of the disease itself and to the treatments. It is observed that these procedures change brain functioning and structure, producing demyelination and various damages that, in one way or another, contribute to the reduction of white matter.
This impairment particularly compromises attention processes and executive functions in children and adolescents.
In executive functions
Regarding executive functions, it is one of the neurocognitive functions most sensitive to radiation and one of the main neuropsychological sequelae of childhood cancer. Being a brain in full developmental maturation, this degeneration of white matter in bilateral prefrontal areas can lead to bradyphrenia (slowing of processing speed), difficulties in problem solving, low cognitive flexibility, planning and organization difficulties, as well as greater difficulty inhibiting responses.
On the other hand, in a very interesting study by Marusak et al. (2019), they report that having been exposed to an experience conceived as a significant objective life threat induces structural and functional changes in the nervous system, even in cases where children had adapted well psychologically to the illness.
This study links cases of Post-Traumatic Stress Disorder in childhood cancer survivors with changes in amygdala volume, showing a centralized, hypersensitive amygdala.
Returning to routine and school
Returning to the child’s routine at home and returning to school are two key scenarios for detecting these possible neuropsychological sequelae of childhood cancer that were not detected during the hospital stage.
It is at this routine stage when they may begin to show learning, memory and literacy difficulties derived from treatments or the type of tumor. For example, after a tumor that has affected the temporal lobes, or if secondary hydrocephalus has occurred, difficulties may arise in acquiring new information or in visuospatial memory.
In addition, in cases where children have undergone oncological treatments at very early ages, there may be a decline in the intellectual capacity expected for their age.
Commonalities
Furthermore, it is common that among the neuropsychological sequelae of childhood cancer there appear difficulties in selective attention (selecting one stimulus over others acting as distractors), alternating (performing two tasks alternately) and sustained (maintaining attentional focus on a task, for example, reading).
Likewise, visuoperceptual difficulties may appear (for example, figure-ground discrimination), sensory recognition difficulties (for example, distinguishing temperature) and dyspraxias (having greater difficulty, for example, acquiring the skill of dressing).
Not all sequelae need to appear at the same time, nor do all currently known ones necessarily have to appear, which is why special attention should be paid to the child’s neurocognitive and emotional functioning during the course of the illness and after cancer treatments in order to carry out the pertinent actions that can help their neurodevelopment if any difference from the child’s pre-treatment functioning is detected.
Conclusion
Due to oncological treatments and many other modulating factors during the course of the illness, there is a high probability of developing neuropsychological sequelae of childhood cancer. This is why it is of utmost importance to recognize them, detect them in time and consult the appropriate professionals to avoid chronicity and thus improve the quality of life of those known as survivors of childhood cancer.
Bibliography
- Bernabeu, J, et al. (2003). Evaluation and neuropsychological rehabilitation in pediatric oncology. Revista de psicooncología, 0, 117-134.
- Hocking, M. C., & Alderfer, M. A. (2012). Neuropsychological sequelae of childhood cancer. Pediatric psycho-oncology: Psychosocial aspects and clinical interventions, 177-186.
- Marusak, H. A., Iadipaolo, A. S., Paulisin, S., Harper, F. W., Taub, J. W., Dulay, K., … & Rabinak, C. A. (2019). Emotion‐related brain organization and behavioral responses to socioemotional stimuli in pediatric cancer survivors with posttraumatic stress symptoms. Pediatric blood & cancer, 66(1), e27470.
- Sohlberg MM, Mateer CA. Attention Process Training (APT). Puyallup, WA: Association for Neuropsychological Research and Development; 1986.
- Zeltzer, L. K., Recklitis, C., Buchbinder, D., Zebrack, B., Casillas, J., Tsao, J. C., … & Krull, K. (2009). Psychological status in childhood cancer survivors: a report from the Childhood Cancer Survivor Study. Journal of clinical oncology, 27(14), 2396.
If you liked this post about neuropsychological sequelae of childhood cancer, you might be interested in these publications from NeuronUP:
“This article has been translated. Link to the original article in Spanish:”
Secuelas neuropsicológicas del cáncer infantil






 Social cognition or how to understand people: social cognition exercises
Social cognition or how to understand people: social cognition exercises
Leave a Reply