Claudia Navarro Pérez, clinical neuropsychologist specialized in tumor neurosurgeries in awake patients, presents in this article all the details about the neurosurgery for brain tumors in awake patients.
What is awake neurosurgery for brain tumors?
Awake neurosurgery for brain tumors, also known as “awake craniotomy”, is one of the most complex and sophisticated techniques in modern medicine, designed to treat certain brain (neurological) diseases, including brain tumors. This technique allows neurosurgeons to perform the surgical removal while ensuring intraoperatively that specific areas of the brain are not damaged, by monitoring in real time while the patient is conscious.
Awake neurosurgery procedure
The procedure is adapted to the characteristics of the tumor, including its size, location and type, as well as the patient’s overall condition.
Before the operation, it will be assessed whether the patient is a candidate for awake neurosurgery, including a series of neurological evaluations and an explanation of the risks and benefits of the specific surgery. If selected, the neuropsychologist will carry out a preoperative assessment to establish the patient’s baseline abilities in different areas. Standardized tests are commonly used to stimulate different brain areas that must be preserved.
During the surgery, brain mapping is performed. The neurosurgeon uses this technique to avoid damaging these areas and to preserve the functions mentioned above. Thus, during intraoperative assessment the neuropsychologist can ask questions or request identification of images and words, count numbers or perform certain movements. The responses provided help the surgeon identify and avoid functional areas in the brain. After the surgery, the specialist will request an MRI to make sure the tumor removal is complete.
After the operation, the patient will remain for several days in the intensive care unit (ICU). Usually, return to routine takes place within a maximum period of between six weeks and three months, during which time the patient will attend regular follow-up appointments with the specialist.
Types of tumors that require awake neurosurgery
Not all brain tumors require the patient to be awake during the surgical procedure. This technique can be applied to:
- Certain primary malignant and metastatic tumors,
- glial tumors (low- and high-grade gliomas),
- cavernomas,
- and arteriovenous malformations near eloquent areas, among others.
Benefits of awake neurosurgery
Awake neurosurgery has notable benefits compared to conventional neurosurgery.
- Firstly, the preservation of neurological functions, since, being awake, the patient can interact with the multidisciplinary team, which helps identify the brain areas to avoid during the operation. Thus, the neurosurgeon can adjust the technique to avoid critical areas and minimize the risk of neurological damage when removing the tumor.
- On the other hand, improved oncological outcomes. Precise access to the tumor allows a total and safe resection, which decreases the likelihood of recurrence and improves the patient’s prognosis.
- Finally, the reduction in recovery time. By avoiding prolonged general anesthesia and associated risks, many patients experience a faster recovery and fewer postoperative complications.

Subscribe
to our
Newsletter
Techniques and tools in awake neurosurgery
Awake neurosurgery requires advanced tools and a highly trained multidisciplinary team. Among the techniques and technologies used are:
Brain mapping
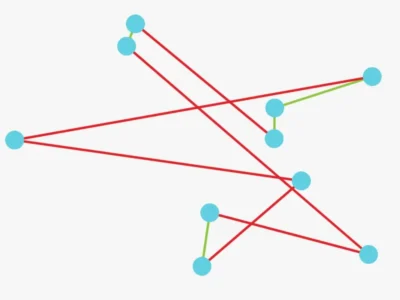
Technique that maps the brain’s functional areas through direct electrical stimulation, which allows surgeons to identify and avoid critical zones thanks to stimulation techniques and identification of cortical structures that may be distorted by the tumor.
Neuronavigation
System that guides the neurosurgeon in real time using three-dimensional images of the brain, providing greater precision and control over the exact location of the tumor.
Intraoperative monitoring
Continuous assessment using stimulation techniques of specific functions such as language or motor skills while the patient performs certain tasks. This helps the team verify that the surgery does not affect these areas. Through stimulation techniques and recordings they evoke responses and continuously monitor in real time during the surgery the functionality of structures near the lesion. Likewise, using a stimulation probe, failures can be induced by responses directly from the cerebral cortex, thus identifying the structures and being able to preserve them.
Direct cortical stimulation
By means of electrical impulses responses are evaluated in the patient, allowing the identification of functional areas with greater precision.
Postoperative care following awake neurosurgery
The recovery from awake neurosurgery is usually faster and less complicated than that of other surgical techniques. Patients generally spend one or two days in the intensive care unit (ICU) for close monitoring and are then transferred to a regular room. Return to routine will depend on the person, but many patients can resume their normal activities within a few weeks.
It is common for patients to experience fatigue and some postoperative discomfort, but many of them, as mentioned above, can resume their normal activities within a few weeks.
Neuropsychological rehabilitation may be necessary to help patients recover affected cognitive and motor functions. In addition, depending on the tumor, additional treatments such as radiotherapy or chemotherapy may be needed to eliminate any residual tumor and reduce the risk of recurrence.
In summary, the prognosis after neurosurgery depends on several factors, including the location and type of the condition treated, as well as the patient’s overall health. However, thanks to this surgical technique, many patients experience a significant improvement in their quality of life, with a reduction of neurological symptoms and complete functional recovery. Regarding rehabilitation and medical follow-up, these are important to ensure an optimal recovery. Advances in surgical technology continue to improve outcomes and prognosis for patients undergoing neurosurgery.
Challenges and advances in awake neurosurgery for brain tumors
Awake neurosurgery for brain tumors faces both technical and human challenges. The need for extreme precision, careful coordination with the medical team and constant communication with the patient require a carefully controlled surgical environment. Despite these challenges, advances in technology and surgical techniques have substantially improved outcomes.
Some recent advances include:
- The advanced imaging: Tools such as functional magnetic resonance imaging and tractography have increased the precision of preoperative planning.
- Augmented reality: Augmented reality allows surgeons to create brain maps in real time, visualizing internal structures while performing the resection.
- The artificial intelligence techniques: They help analyze large volumes of patient data and facilitate better personalization of procedures, adapting to the specific characteristics of each case.
Advanced neuroimaging techniques
The diagnosis of brain tumors has improved significantly with the introduction of advanced neuroimaging techniques:
- Magnetic resonance imaging (MRI) with its functional modalities and positron emission tomography (PET) allow specialists not only to identify the presence of a tumor, but also to assess its metabolism, aggressiveness and its impact on critical areas of the brain.
- MR spectroscopy, for example, helps differentiate between tumor tissue and post-surgical scarring, while tractography allows visualization of neural pathways to plan the surgery.
- One of the most promising developments in the field of neuro-oncology is image-assisted neuronavigation. This tool uses three-dimensional models based on preoperative images to guide neurosurgeons during the intervention, increasing precision and reducing the risk of damage to critical brain areas.
- Likewise, the use of liquid biomarkers, such as the detection of circulating tumor DNA in cerebrospinal fluid, is emerging as a non-invasive method to monitor disease progression and response to treatment.
Through technological advances, modern surgical techniques in neurosurgery have significantly reduced risks and improved outcomes for patients. By allowing greater precision, they minimize damage to healthy brain tissue. In addition, postoperative recovery is faster and with fewer complications.
Conclusion
Awake neurosurgery for brain tumors is a safe and effective option to treat tumors in sensitive areas of the brain. Thanks to its ability to preserve neurological functions and minimize impact on the patient’s quality of life, this technique is becoming the standard of care for certain brain tumors. With continuous advances in technologies and techniques, the future of awake neurosurgery promises even more precision and safety, offering renewed hope for patients with brain tumors in critical areas.
Bibliography
- Abdulrauf SI, Urquiaga JF, Patel R, Albers JA, Sampat VB, Baumer M, et al. Awake microvascular decompression for trigeminal neuralgia: concept and initial results. World Neurosurg. 2018;113: e309-e313.
- Barbara Woodward Lips Patient Education Center. Surgical treatment for seizures. Rochester, Minn.: Mayo Foundation for Medical Education and Research; 2004.
- Brydges G, et al. Awake craniotomy: A practice overview. American Association of Nurse Anesthetists. 2012;80:61.
- Huncke K, Van de Wiele B, Fried I, Rubinstein EH. The asleep-awake-asleep anesthetic technique for intraoperative language mapping. Neurosurgery. 1998;42:1312-1316.
- Jaramillo MJ. Anesthesia for awake craniotomy. Rev Mex Anest. 2009;32:S77-S78.
- Meng L, McDonagh DL, Berger MS, Gelb AW. Anesthesia for awake craniotomy: a how-to guide for the occasional practitioner. Can J Anaesth. 2017;64:517-529.
- Ramírez-Segura EH. Anesthesia for awake craniotomy: asleep-awake-asleep technique. Rev Mex Anest. 2014;37:48-52.
- Riggin, EA. Allscripts EPSi. Mayo Clinic, Rochester, Minn. June 26, 2016.
If you enjoyed this blog post about awake neurosurgery for brain tumors: procedure, benefits, and advances, you will likely be interested in these NeuronUP articles:
“This article has been translated. Link to the original article in Spanish:”
Neurocirugía para tumores cerebrales con paciente despierto: procedimiento, beneficios y avances






 Current trends in the treatment of mental illnesses
Current trends in the treatment of mental illnesses
Leave a Reply