María José García Rubio, Doctor in Clinical and Health Psychology, explains in this article what hydrocephalus is and how to apply a cognitive stimulation program to this disorder.
What is hydrocephalus?
Pediatric hydrocephalus is an urgent neurodevelopmental disorder worldwide because of its consequences and because of the high incidence sustained by low-income countries such as many that make up East and Southern Africa.
Specifically, the 10,000 cases of infant hydrocephalus recorded per year worldwide compete with the 200,000 cases of hydrocephalus recorded in this population in Africa alone.
Hydrocephalus involves an excess of cerebrospinal fluid (CSF) in the brain before birth, although there are also cases where hydrocephalus was caused during delivery or even after it.
As its name indicates, the term “hydrocephalus” arises from the combination of the Greek words for “water” and “head”. In this specific case, the “water” would be the CSF that supports and protects the brain in such a way that if it accumulates due to a deficit in the brain it generates disproportionate pressure.
Although the focus of this post is on how cognitive stimulation is linked to pediatric hydrocephalus, the origin of the disorder is briefly described below to better understand the associated cognitive treatment.
What is the function of CSF?
As anticipated above, the excess of CSF is the key factor in hydrocephalus. In this sense, it is worth remembering that the central nervous system (CNS) is made up of the brain and the spinal cord.
The CNS is essential for complex tasks such as perception, performing voluntary and involuntary movements, language expression and production, emotions, and other cognitive abilities such as memory, attention, planning and/or inhibition, among many others.
Because of its complexity, the CNS has other support systems such as the ventricular system, whose main function is to maintain appropriate circulation of the CSF on which the brain floats.
Likewise, the CSF is produced by the choroid plexus, a network of cells that extends throughout the ventricles. In people without hydrocephalus, CSF flows from the plexus to the ventricles to nourish and support the cells of the CNS.
In the pediatric population with hydrocephalus this process is interrupted, that is, there is a kind of “blockage” and hence the excess of CSF.
But why does this interruption of flow occur in cases of hydrocephalus?
There are several causes for infant hydrocephalus, one of the most common being aqueductal stenosis. This is a condition in which there is a narrowing of the canal that connects the four ventricles, so the CSF stops flowing.
Likewise, hydrocephalus can be the consequence of other disorders such as spina bifida and/or myelomeningocele. In addition, hydrocephalus can also be acquired, that is, caused by an accident involving head trauma for example.
What is the neuropsychological profile of hydrocephalus?
So far there is no specific profile of the child patient with hydrocephalus because the incidence, at least in middle- to high-income countries, is not high, which means the disorder is studied less.
However, there is literature on the neuropsychological consequences that appear after infant hydrocephalus in low-income countries.
Overall, motor impairments have been shown to be the most frequent in this population. This can be explained based on the extent of the motor cortex and the implication that excess CSF has on it.
Along with the worsening of motor skills it has been observed that the pediatric population with hydrocephalus has a greater predisposition to a low intelligence quotient (IQ), and perceptual and sensory problems such as partial loss of vision or hearing.
Other studies have concluded that the profile associated with infant hydrocephalus is heterogeneous with impairment in memory, attention and planning. Regarding language, there is consensus in considering it the most preserved cognitive domain in pediatric hydrocephalus patients, although more research is needed on this matter.
Given the heterogeneity of the neuropsychological profile associated with hydrocephalus, what impact would the application of a cognitive stimulation program have on this population?
Cognitive stimulation is the set of techniques and tools applied to improve a patient’s cognitive performance, through direct intervention on their abilities such as memory, attention, and language, among others.
In general, the application of this type of stimulation responds to specific requirements linked to the type of diagnosis and the patient’s cognitive deficit observed after the neuropsychological evaluation.
In infant hydrocephalus, implementing a cognitive stimulation program is not an easy task; this is due especially to the heterogeneity that hydrocephalus implies in neuropsychological terms.
In fact, to date authors have not reached a consensus on the cognitive stimulation protocol to follow in the pediatric hydrocephalus population.
In these cases, professionals apply different cognitive tasks adapted to the deficit, age and severity of the hydrocephalus, among other factors. However, there are some indicators that have proven effective in clinical practice.
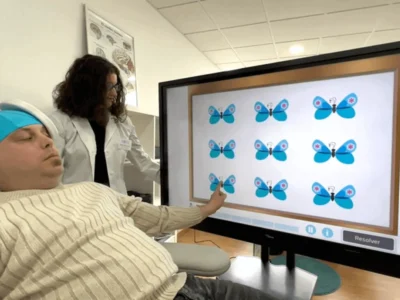
For memory stimulation many professionals use digital tasks on platforms such as NeuronUP involving recognition of similar objects, and the spontaneous retrieval of previously learned stimuli.
Attention, on the other hand, is also one of the domains most stimulated in infant hydrocephalus. In most cases attention is stimulated through tasks that involve sustained and selective attention such as visual search, or “spot the differences” activities.
In sum, planning is another area that benefits patients with hydrocephalus if appropriate cognitive stimulation is provided.
In this regard, they are usually asked to break down some tasks or routines (for example, the steps they take to get dressed and/or have breakfast), or that through digital tasks they are able to create a plan, follow it and achieve the objective.
Finally, stimulation of the sensorimotor abilities that are affected in the vast majority of cases of infant hydrocephalus is recommended. For this stimulation professionals usually resort to exercises that involve sensory detection and conscious perception, for example.
In the case of motor stimulation, the focus is on voluntary and involuntary movements to achieve the initiation of voluntary walking, control of muscle tone and movements, and/or balance, among other motor milestones.
Conclusion
In summary, the cognitive stimulation exercises proposed here are good recommendations to start working with child patients with hydrocephalus, at least in the first sessions.
However, it is important to emphasize that each cognitive stimulation program must be adapted to the patient’s conditions, which in turn are subordinated to the type, severity, and age at diagnosis of the hydrocephalus.
Bibliography
Bannink Mbazzi, F., Fontaine, J., Idro, R., & Van Hove, G. (2016). Cognitive abilities of pre-and primary school children with spina bifida in Uganda. International Journal of Educational Psychology, 5(3), 249-280. 10.17583/ijep.2016.2075
Işık, U., Özek, M.M. (2019). Clinical Findings of Children with Hydrocephalus. In: Cinalli, G., Özek, M., Sainte-Rose, C. (eds) Pediatric Hydrocephalus. Springer, Cham. https://doi.org/10.1007/978-3-319-27250-4_46
Kahle, K. T., Kulkarni, A. V., Limbrick, D. D., & Warf, B. C. (2016). Hydrocephalus in children. The lancet, 387(10020), 788-799. https://doi.org/10.1016/S0140-6736(15)60694-8
Lin, C. T., & Riva-Cambrin, J. K. (2015). Management of posterior fossa tumors and hydrocephalus in children: a review. Child’s Nervous System, 31, 1781-1789. https://doi.org/10.1007/s00381-015-2781-8
Paturu, M., Triplett, R. L., Thukral, S., Alexopoulos, D., Smyser, C. D., Limbrick, D. D., & Strahle, J. M. (2021). Does ventricle size contribute to cognitive outcomes in posthemorrhagic hydrocephalus? Role of early definitive intervention. Journal of Neurosurgery: Pediatrics, 29(1), 10-20. https://doi.org/10.3171/2021.4.PEDS212
Rekate, H. L., & Blitz, A. M. (2016). Hydrocephalus in children. Handbook of clinical neurology, 136, 1261-1273. https://doi.org/10.1016/B978-0-444-53486-6.00064-8
Riva-Cambrin, J., Kulkarni, A. V., Burr, R., Rozzelle, C. J., Oakes, W. J., Drake, J. M., … & Kestle, J. R. (2021). Impact of ventricle size on neuropsychological outcomes in treated pediatric hydrocephalus: an HCRN prospective cohort study. Journal of Neurosurgery: Pediatrics, 29(3), 245-256. https://doi.org/10.3171/2021.8.PEDS21146
Rizvi, R., & Anjum, Q. (2005). Hydrocephalus in children. JPMA. The Journal of the Pakistan Medical Association, 55(11), 502-507.
Zielińska, D., Rajtar-Zembaty, A., & Starowicz-Filip, A. (2017). Cognitive disorders in children’s hydrocephalus. Neurologia i neurochirurgia polska, 51(3), 234-239. https://doi.org/10.1016/j.pjnns.2017.02.001
If you liked this article about educational inclusion and how to work on it with NeuronUP, you might also be interested in the following articles:
“This article has been translated. Link to the original article in Spanish:”
Estimulación cognitiva en niños con hidrocefalia





 Worksheet for working on selective attention in adults: Counting and Selecting
Worksheet for working on selective attention in adults: Counting and Selecting
Leave a Reply