Neuropsychology expert Cristina Troyano Jiménez explains in this article what frontotemporal dementia is, its types, symptoms, causes, diagnosis and treatment.
What is frontotemporal dementia
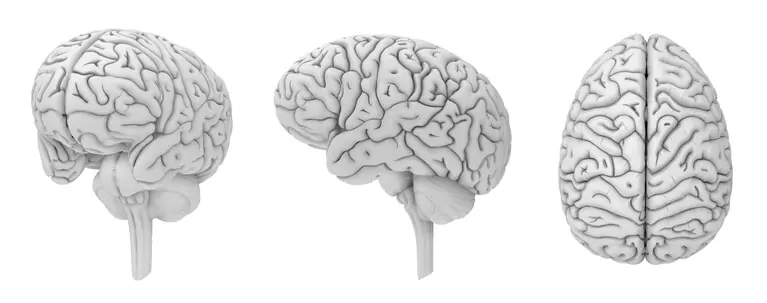
Frontotemporal dementia (FTD) is a dementia with a lower incidence and it affects younger people (40-65). It is the second cause of presenile dementia, the involvement is in the frontal and temporal lobes (they atrophy).
The symptoms that most commonly appear are mainly behavioral and personality-related. Patients with frontotemporal dementia can become complex to manage. They can create numerous conflicts by having personality changes, leading to confrontations with others and even with their relatives.
Types of frontotemporal dementia
Frontotemporal dementia affects the frontal and temporal lobes, causing atrophy of these. Unlike other dementias, the involvement produces changes in behavior, problems with language and speech and in some cases movement disorders.
Frontotemporal dementia with behavioral problems:
In these patients personality changes appear. Their behavior changes; they may become very agitated or, on the contrary, so inhibited that if not prompted they would not move from where they are.
Among personality changes we find disinhibition and increasingly inappropriate behaviors:
- They neglect their hygiene
- In some, interest in sex increases, with some even developing Klüver-Bucy syndrome (greater interest in sex, lip smacking and putting objects in the mouth…)
- Their language may become more obscene
- They may have repetitive behaviors
- They can become more impulsive or compulsive
Frontotemporal dementia with aphasia:
In these cases the language area is the most affected, and they have problems speaking, communicating, reading, writing and understanding.
They begin with language deficits such as anomia and articulation problems, etc., and progress until communication is nil; language symptoms can be the only ones for years in this dementia. In other cases progression is faster. As the disease advances they tend to speak less until they stop speaking.
Frontotemporal dementia with movement disorders:
There is involvement of movement, which can lead to FTD with parkinsonism or FTD with amyotrophic lateral sclerosis.
One type of frontotemporal dementia is Pick’s disease, which is characterized by severe atrophy, cell death and the presence of abnormal Pick cells.
Symptoms of frontotemporal dementia
- They are progressive, but the course varies among patients
- They affect personality, behavior and language
- Memory involvement is less than in other dementias
- Difficulties in abstract thinking, attention and recent memory
- Planning and organization to carry out tasks or develop ideas
are affected - They are easily distracted, but are usually oriented and perform activities of daily
living - Dysarthria or difficulty articulating speech
- Those with aphasia often have weakness in the muscles of the head and neck
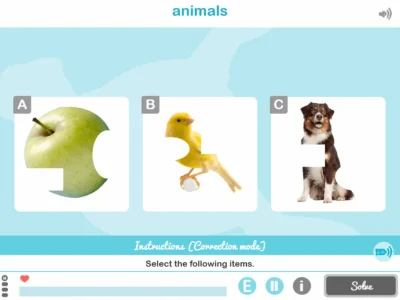
and hence impairment in swallowing - Anomia may appear (not recognizing objects) and prosopagnosia (not recognizing
faces)
Causes of frontotemporal dementia
The causes of frontotemporal dementia are not fully known, although it is true that patients with this condition present greater amounts or abnormal forms of the proteins TAU and TDP-43 in neurons, with the accumulation of these causing damage and consequent cell death.
In other cases there seems to be a genetic mutation; there appears to be a relationship between the behavioral variant and this cause, and it is believed that between 10 and 30% of patients with frontotemporal dementia have this. It has also been shown that with a family history of FTD, there is a genetic cause.
Diagnosis of frontotemporal dementia
The diagnosis of frontotemporal dementia is complex, since the symptoms can be confused with other dementias, and it is not uncommon for it to initially be misdiagnosed as Alzheimer-type dementia. Being a less frequent and less known dementia, in these cases the medication is also incorrect.
This leads us to the great importance of an accurate diagnosis. For years I have observed such cases and the medication did not act on the symptoms, with symptoms remitting when the diagnosis and pharmacology were correct. Nowadays, fortunately we have sufficient neuroimaging techniques that are capable of showing where the brain is affected and corroborate the diagnosis.
Among the most novel neuroimaging techniques are brain magnetic resonance imaging and cortical mean diffusivity, which help us achieve a more exact diagnosis.
The diagnosis of frontotemporal dementia is usually initially made with the clinical interview of the patient and their relatives, complemented with neuroimaging tests; in some cases suspected to be hereditary, a genetic test would confirm it.
Unfortunately, one way to confirm it is a posteriori, by brain autopsy, as in almost all dementias.
Treatments for frontotemporal dementia
Pharmacological treatment
As pharmacological treatment there is the use of antipsychotics for patients with behavioral problems, especially compulsive behaviors. Also the use of antidepressants and in the case of movement problems, the use of medications that act in that area.
Among the new treatments that have been put into practice is Sodium Selenate, which increases the enzyme protein phosphatase 2A, which breaks down the TAU protein, which we see in neurons in large quantities in patients with dementia.
Non-pharmacological treatment
As non-pharmacological treatment, there is a variety, depending on the type of patient.
For patients with language problems, it is important to see a speech therapist.
For patients with movement problems, physiotherapy is recommended.
And in general the use of occupational therapy and cognitive stimulation, although it is true that compared with other dementias, orientation and memory are not as affected initially, it is important to work all brain areas.
And above all it is important for these patients to have a daily routine.
Progression of frontotemporal dementia
The progression of frontotemporal dementia is different from other dementias, such as Alzheimer’s. It is usually progressive and depends on each patient.
In some, the progression is slower, around ten years, and in others it is faster; the type of lesion influences this. For example, a patient with aphasia will eventually develop swallowing problems such as dysphagia and their course will be totally different from that of a patient with mobility or behavioral problems.
The behavioral variant is the one that advances fastest, the aphasia variant has an intermediate course.
Average life expectancy is between 6 and 8 years, maximum 15 years.
What is important, as with all dementias, apart from an early and accurate diagnosis, is to address it as soon as possible through different options: cognitive stimulation, physiotherapy, occupational therapy, etc.
I have been working in this area for many years and have seen patients of all kinds. I have also seen how all these techniques have made the disease progress more slowly. However, it is true that in the last three years, during the pandemic, many patients stopped going to day centers and their progression was faster. Healthcare somewhat sidelined specialties, with COVID-19 protocols, and many have been diagnosed at an advanced stage; both pharmacological and non-pharmacological treatment arrive late and we find very advanced patients, often with behavioral problems. Working with them becomes complicated. These are some of the collateral problems of a pandemic in which everything was paralyzed.
Conclusions
Frontotemporal dementia, like many dementias, is a psychosocial disease, since it not only affects the patient but also their surroundings, caregivers and family members.
Perhaps right now we are reaching the peak of this silent pandemic which, together with the aging of the population we are experiencing, affects more and more people. Much progress has been made both in the causes, medication, technology, diagnosis and in day-to-day coping (through the different therapies).
There is still a way to go. Undoubtedly, advances in genetic engineering and technology will help in the future for a very early diagnosis and even so that one day they may be eradicated, like many diseases in the past. But in the present we continue day by day, combating the disease with the means we have and trying to give the patient and their environment quality of life and dignity.
Alzheimer’s erases memory, not feelings.
Pascual Maragall
Frequently asked questions about frontotemporal dementia
1. What is frontotemporal dementia?
Frontotemporal dementia (FTD) is a neurodegenerative disorder that atrophies the frontal and temporal lobes. It usually begins between 40 and 65 years and mainly causes behavioral and language alterations. It is an important cause of presenile dementia.
2. What are the types of frontotemporal dementia?
There are three main presentations: behavioral variant (personality changes and disinhibition), FTD with aphasia (language impairment) and FTD with movement disorders (parkinsonism or ALS). Pick’s disease is a subtype with severe atrophy and Pick cells.
3. What symptoms does frontotemporal dementia cause?
It causes personality changes, disinhibition and impulsivity, repetitive behaviors and problems planning and organizing. Language may become obscene or impoverished; there is dysarthria, anomia and prosopagnosia. Memory is usually less affected than in other dementias.
4. What are the causes of frontotemporal dementia?
It is associated with abnormal accumulation of tau and TDP-43 proteins in neurons, leading to damage and cell death. In 10–30% there are genetic mutations and family history, especially in the behavioral variant.
5. How is frontotemporal dementia diagnosed?
The diagnosis combines clinical and family interview with neuroimaging. Magnetic resonance imaging and cortical mean diffusivity help to locate the atrophy. In suspected hereditary cases genetic tests are requested. Definitive confirmation can be performed post mortem.
6. What treatments exist for frontotemporal dementia?
There is no cure. Management includes antipsychotics for compulsive behaviors, antidepressants and drugs for movement disorders. Speech therapy, physiotherapy, occupational therapy, cognitive stimulation and daily routines are recommended. Sodium selenate is being studied for its action on tau.
References
- Parkin, A. (2003). Explorations in Neuropsychology, Editorial Médica Panamericana.
- Carpintero H, Delius J, Fierro A, León Carrión A. (2001), Cognitive Neuropsychology, some current problems. Ediciones Aljibe.
- HYPERLINK “https://www.msdmanuals.com/es-es/hogar/authors/huang-juebin” ‘Juebin Huang’, MD, PhD, Department of Neurology, University of Mississippi Medical Center. Last complete review Mar. 2021.
- https://www.mayoclinic.org/es-es/diseases-conditions/frontotemporal-dementia/diagnosis-treatment/drc-20354741.2022
- https://www.alzheimers.gov/es/alzheimer-demencias/demencia-frontotemporal.2022
If you liked this article about frontotemporal dementia, you may also be interested in the following articles:
“This article has been translated. Link to the original article in Spanish:”
Demencia frontotemporal: qué es, tipos, síntomas, causas, diagnóstico y tratamiento



 Worksheet to stimulate working memory in children: The Correct Order
Worksheet to stimulate working memory in children: The Correct Order
Leave a Reply