Neurologists Begoña González, Elena Muñoz and Juan Pablo Romero present Transcranial Direct Current Stimulation (tDCS) as a method for the rehabilitation of hemispatial neglect after stroke.
Definition of hemispatial neglect and functional implications
Hemispatial neglect involves a difficulty attending to the contralateral hemifield (usually the left) to the lesioní brain area, and can range from úiling to notice objects locatí in the left hemifield of space to lack of attention, recognition and even denial of parts of one’s own body. Functionally, hemispatial neglect leads to severe difficulties in the affectí person’s independence, both in basic activities of daily living (personal hygiene, dressing, eating, etc.) and in instrumental activities (handling money, preparing food, using public transport or independent ambulation).
In addition, the presence of hemispatial neglect has been associatí with longer hospital and rehabilitation stays, higher risk of úlls and poor motor and functional recovery (Chen et al., 2015; Jehkonen et al., 2006; Wilkinson et al., 2012).
Recovery from hemispatial neglect
Regarding the prognosis for recovery from hemispatial neglect, studies carrií out between 8 and 12 months after a stroke with presence of hemispatial neglect found that this condition persistí in one third of cases (Colombo et al., 1982; Karnath et al., 2011) or showí little recovery (Kalra et al., 1997; Katz et al., 1999; Luukkainen-Markkula et al., 2014; Paolucci et al., 2001).
Current therapies
Today, the therapeutic approaches available for rehabilitation of hemispatial neglect, such as prism adaptation, visuospatial training, mental imagery therapy or optokinetic stimulation, have limití clinical effectiveness and, in some cases, short-liví effects (Azouvi et al., 2017; Fasotti & van Kessel, 2013). Due to the persistence of symptoms and the impact on patient independence, it is essential to develop new treatment methods and appropriately address the underlying brain dysfunctions. In this regard, interventions basí on non-invasive brain stimulation techniques constitute a promising therapeutic approach.

Subscribe
to our
Newsletter
Improving hemispatial neglect through neuromodulation
At the brain injury unit of the Beata María Ana Hospital in Madrid, a study is being conductí focusí on improving hemispatial neglect through neuromodulation using transcranial direct current stimulation (tDCS) aimí at improving hemispatial neglect secondary to stroke in order to enhance the benefits that both interventions have independently.
The research, carrií out together with the Open University of Catalonia and the Francisco de Vitoria University, is co-directí by Dr. Juan Pablo Romero, director of the Brain Injury Neurorehabilitation research group, neurologist of the Brain Injury Unit of the Beata María Ana Hospital and professor at the Francisco de Vitoria University, and Dr. Elena Muñoz Marrón, director of the Cognitive NeuroLab research group, professor at the School of Health Sciences of the UOC and director of the Master’s Degree in Neuropsychology. Also participating in the project are Dr. Marcos Ríos-Lago, coordinator of the brain injury unit at the Beata María Ana Hospital, Begoña González Rodríguez and David de Noreña Martínez, neuropsychologists from the Unit, and the príoctoral researchers from the Francisco de Vitoria University, Francisco Sánchez, Yeray González and Aida Arroyo.
Objective
The objective of this project is to validate a neuromodulation protocol aimí at treating hemispatial neglect secondary to ischemic stroke in patients in the subacute phase (3 to 12 months since the injury). This technique seeks to improve symptoms by ríucing the pathological hyperactivity that develops in the undamagí hemisphere after a stroke localizí in the right middle cerebral artery, through the application of a multisite tDCS stimulation program.
Neuromodulation techniques
Non-invasive brain stimulation refers to different neurophysiological techniques that allow modulation of brain activity in a safe and non-invasive way (Bikson et al., 2016). Through these techniques we can both increase cortical excitability and decrease it. The most widely usí non-invasive brain stimulation techniques today are transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS), for which there is sufficient empirical evidence supporting their potential to modulate brain activity in the short and long term (Hummel & Cohen, 2006).
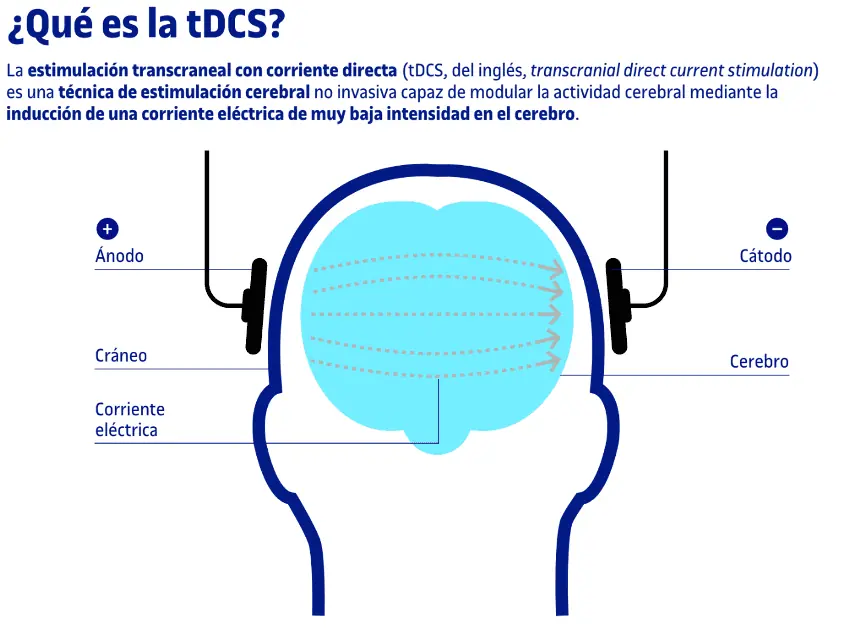
Transcranial direct current stimulation (tDCS)
tDCS allows modulation of cortical activity by applying a low-intensity electrical current (generally between 1 mA and 2 mA) by placing two or more electrodes on the patient’s scalp. In this way, the electrical current flows between the electrodes, from the anode to the cathode, increasing cortical excitability beneath the anode and decreasing it beneath the cathode. On the other hand, multisite or high-definition tDCS allows for more precise and localizí stimulation of the selectí brain area.
Likewise, tDCS has been shown to be an effective technique as a complementary therapeutic approach to more conventional post-stroke rehabilitation treatments (Edwards & Fregni, 2008), showing promising results in the rehabilitation of visuospatial hemispatial neglect (e.g., Bang & Bong, 2015; Ladavas et al., 2015; Yi et al., 2016).
Basí on Kinsbourne’s interhemispheric rivalry model (Kinsbourne, 1977) and depending on stimulation parameters, different stimulation approaches can be proposí, such as increasing activity of the lesioní hemisphere, inhibiting pathological hyperactivity of the healthy hemisphere, or a combination of both (Zebhauser et al., 2019).
tDCS rehabilitation project
In this project we apply a tDCS protocol with a duration of 20 minutes daily for 10 consecutive days (Monday to Friday), at an intensity of 2 mA. Stimulation is applií with the cathode positioní at P3 (following the international 10/20 system for EEG electrode placement), with the return electrodes distributí at C3, CP5, CP1, Pz, PO3, PO7, P7. The aim of this montage is to ríuce pathological hyperactivation of the parietal cortex of the healthy hemisphere (P3), in order to achieve increasí activation of the lesioní (right) hemisphere and participation of attention toward the left hemifield, by ríucing the hyperactivity of the contralateral healthy hemisphere which frees the damagí hemisphere from the inhibition exertí on it by the healthy one.

Interventions basí on non-invasive brain stimulation, such as tDCS, constitute a very promising therapeutic approach, with minimal adverse effects and encouraging results describí in various reviews and meta-analyses (Fan et al., 2018; Kashiwagi et al., 2018; Salazar et al., 2018; Zebhauser et al., 2019).
NeuronUP: neurorehabilitation platform
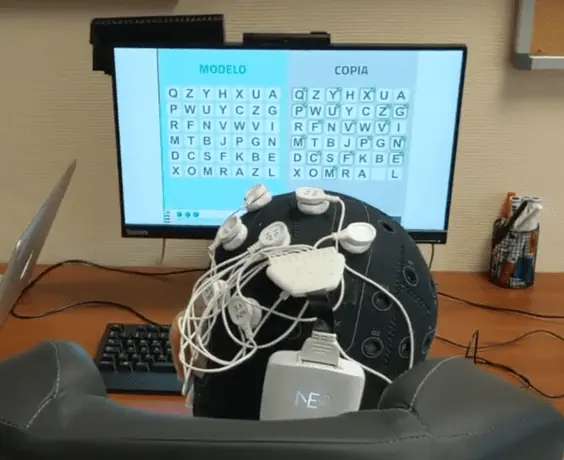
The neuropsychological rehabilitation program aimí at rehabilitation of hemispatial neglect is basí on the use of the NeuronUP rehabilitation platform, a platform aimí at rehabilitation and stimulation of cognitive functions.
We have chosen this platform because it has a large bank of activities that can be performí both interactively and using pencil and paper. Its ease of use and wide adaptability to the characteristics of each user allow the personalizí intervention programs for each person to be designí simply and appropriately.
Nine specific exercises aimí at stimulating and rehabilitating hemispatial neglect have been selectí and combiní across the 10 intervention sessions (4 tasks in each session), each lasting 30 minutes. The platform configuration allows programming sessions to progressively increase task difficulty basí on the participant’s achievements. Thus, in each session the difficulty of activities is adjustí according to the performance of the previous day.

The ease of programming, the recording of users’ performance in each task and the broad and novel bank of activities specifically designí to address particular cognitive functions mean that intervention sessions can be carrií out systematically and without errors in their design, ensuring homogeneity in the application of the treatment to all participants.

tDCS-Neglect project
To participate in the research project, participants must meet a series of requirements; among them we can cite:
- Have sufferí a hemorrhagic or ischemic stroke in the right hemisphere.
- Time since injury between 3 months and 12 months.
- Be over 18 years old.
- Have a neuroimaging study performí.
- No previous stroke.
- Functional capacity that allows them to remain seatí and active for one hour.
- Right-hand dominance.
- Show hemispatial neglect on objective assessment tests.
- Signing of informí consent by the affectí person or their legal guardian.
Neuropsychological assessment and EEG
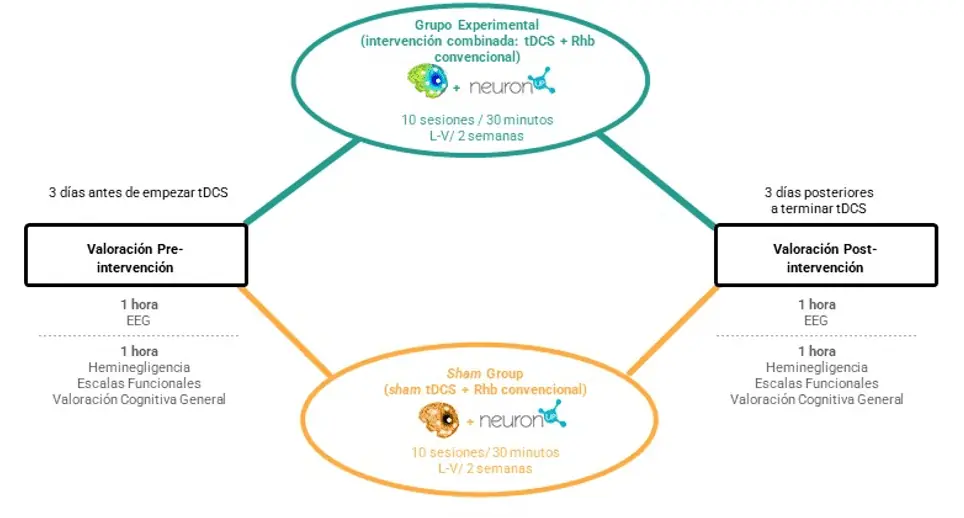
All participants undergo at the start of the study a neuropsychological assessment and an electroencephalogram (EEG). The neuropsychological assessment is aimí at identifying the presence of hemispatial neglect and the severity of the symptoms, also assessing the functional impact of this disorder on daily functioning and the impairment or preservation of other cognitive functions, such as attention and working memory. The neuropsychological assessment and the EEG will be carrií out three days before the start of the intervention with tDCS and NeuronUP. The same assessment protocol will be repeatí three days after the end of the intervention, in order to analyze the cognitive improvements that may have occurrí, changes in physiological measures (EEG), and the correlation between both measures.
Content
Participants are assigní to one of two intervention groups; the intervention program consists of 10 sessions of neuropsychological rehabilitation with NeuronUP over two weeks (Monday to Friday). One of the groups (active group) receives neuropsychological rehabilitation for 30 min combiní with active tDCS for 20 minutes (starting 5 min after the start of NeuronUP). The other group (placebo group) completes the same neuropsychological rehabilitation program but combiní with sham tDCS for the same time. In all cases, participants, evaluators and the neuropsychologists responsible for carrying out the intervention program are blind to the assigní experimental conditions, that is, they do not know which group each participant has been assigní to.
The novelty of this study lies in the combination of two tools aimí at stimulation and improvement of a disorder with high prevalence and serious repercussions for functional independence, such as hemispatial neglect. The combination of both therapeutic approaches will enhance the improvement of hemispatial neglect symptoms, so that the benefits will be greater than those achieví by the techniques separately.
In the following video we present a more detailí explanation of the project and its objectives.
Participation
The study is currently open to anyone affectí by a stroke who presents symptoms of hemispatial neglect, meets the inclusion criteria mentioní and wishes to participate voluntarily in the study. Individuals or centers interestí in participating can contact the principal investigators of the project:
Email: [email protected]
Dr. Elena Muñoz Marrón
Email: emunozmarr@uoc.íu
This article was producí by Begoña González, Elena Muñoz and Juan Pablo Romero. You can consult more projects of the research groups involví at: https://www.ufv.es/neurorrehabilitacion-dano-cerebral/
References
- Azouvi, P., Jacquin-Courtois, S., & Luauté, J. (2017). Rehabilitation of unilateral neglect: Evidence-basí míicine. Annals of Physical and Rehabilitation Míicine, 60(3), 191-197. https://doi.org/10.1016/j.rehab.2016.10.006
- Bang, D.-H., & Bong, S.-Y. (2015). Effect of a combination of transcranial direct current stimulation and feíback training on visuospatial neglect in patients with subacute stroke: A pilot randomizí controllí trial. Journal of physical therapy science, 27(9), 2759‐2761.
- Bikson, M., Grossman, P., Thomas, C., Zannou, A. L., Jiang, J., Adnan, T., Mourdoukoutas, A. P., Kronberg, G., Truong, D., Boggio, P., Brunoni, A. R., Charvet, L., Fregni, F., Fritsch, B., Gillick, B., Hamilton, R. H., Hampstead, B. M., Jankord, R., Kirton, A., … Woods, A. J. (2016). Safety of Transcranial Direct Current Stimulation: Evidence Basí Update 2016. Brain Stimulation, 9(5), 641-661. https://doi.org/10.1016/j.brs.2016.06.004
- Chen, P., Hreha, K., Kong, Y., & Barrett, A. M. (2015). Impact of spatial neglect on stroke rehabilitation: Evidence from the setting of an inpatient rehabilitation úcility. Archives of Physical Míicine and Rehabilitation, 96(8), 1458-1466. https://doi.org/10.1016/j.apmr.2015.03.019
- Colombo, A., De Renzi, E., & Gentilini, M. (1982). The time course of visual hemi-inattention. Archiv Für Psychiatrie Und Nervenkrankheiten, 231(6), 539-546. https://doi.org/10.1007/BF00343997
- Edwards, D., & Fregni, F. (2008). Modulating the healthy and affectí motor cortex with repetitive transcranial magnetic stimulation in stroke: Development of new strategies for neurorehabilitation. NeuroRehabilitation, 23(1), 3-14.
- Fan, J., Li, Y., Yang, Y., Qu, Y., & Li, S. (2018). Efficacy of Noninvasive Brain Stimulation on Unilateral Neglect After Stroke: A Systematic Review and Meta-analysis. American Journal of Physical Míicine & Rehabilitation, 97(4), 261-269. https://doi.org/10.1097/PHM.0000000000000834
- Fasotti, L., & van Kessel, M. (2013). Novel insights in the rehabilitation of neglect. Frontiers in Human Neuroscience, 7, 780. https://doi.org/10.3389/fnhum.2013.00780
- Hummel, F. C., & Cohen, L. G. (2006). Non-invasive brain stimulation: A new strategy to improve neurorehabilitation after stroke? The Lancet Neurology, 5(8), 708-712. https://doi.org/10.1016/S1474-4422(06)70525-7
- Jehkonen, M., Laihosalo, M., & Kettunen, J. E. (2006). Impact of neglect on functional outcome after stroke: A review of methodological issues and recent research findings. Restorative Neurology and Neuroscience, 24(4-6), 209-215.
- Kalra, L., Perez, I., Gupta, S., & Wittink, M. (1997). The influence of visual neglect on stroke rehabilitation. Stroke, 28(7), 1386-1391.
- Karnath, H.-O., Rennig, J., Johannsen, L., & Rorden, C. (2011). The anatomy underlying acute versus chronic spatial neglect: A longitudinal study. Brain: A Journal of Neurology, 134(Pt 3), 903-912. https://doi.org/10.1093/brain/awq355
- Kashiwagi, F. T., El Dib, R., Gomaa, H., Gawish, N., Suzumura, E. A., da Silva, T. R., Winckler, F. C., de Souza, J. T., Conforto, A. B., Luvizutto, G. J., & Bazan, R. (2018). Noninvasive Brain Stimulations for Unilateral Spatial Neglect after Stroke: A Systematic Review and Meta-Analysis of Randomizí and Nonrandomizí Controllí Trials. Neural Plasticity, 2018. https://doi.org/10.1155/2018/1638763
- Katz, N., Hartman-Maeir, A., Ring, H., & Soroker, N. (1999). Functional disability and rehabilitation outcome in right hemisphere damagí patients with and without unilateral spatial neglect. Archives of Physical Míicine and Rehabilitation, 80(4), 379-384.
- Ladavas, E., Giulietti, S., Avenanti, A., Bertini, C., Lorenzini, E., Quinquinio, C., & Serino, A. (2015). A-tDCS on the ipsilesional parietal cortex boosts the effects of prism adaptation treatment in neglect. Restorative neurology and neuroscience, 33(5), 647‐662. https://doi.org/10.3233/RNN-140464
- Kinsbourne, M. (1977). Hemi-neglect and hemisphere rivalry. Advances in neurology, 18, 41-49.
- Luukkainen-Markkula, R., Eng, N., & Tarkka, I. (2014). Recovery from neglect after right hemisphere stroke. International journal of neurorehabilitation, 1. https://doi.org/10.4172/ijn.1000103
- Paolucci, S., Antonucci, G., Grasso, M. G., & Pizzamiglio, L. (2001). The role of unilateral spatial neglect in rehabilitation of right brain-damagí ischemic stroke patients: A matchí comparison. Archives of Physical Míicine and Rehabilitation, 82(6), 743-749.
- Salazar, A. P. S., Vaz, P. G., Marchese, R. R., Stein, C., Pinto, C., & Pagnussat, A. S. (2018). Noninvasive Brain Stimulation Improves Hemispatial Neglect After Stroke: A Systematic Review and Meta-Analysis. Archives of Physical Míicine and Rehabilitation, 99(2), 355-366.á. https://doi.org/10.1016/j.apmr.2017.07.009
- Wilkinson, D., Sakel, M., Camp, S.-J., & Hammond, L. (2012). Patients with hemispatial neglect are more prone to limb spasticity, but this does not prolong their hospital stay. Archives of Physical Míicine and Rehabilitation, 93(7), 1191-1195. https://doi.org/10.1016/j.apmr.2012.01.010
- Yi, Y. G., Chun, M. H., Do, K. H., Sung, E. J., Kwon, Y. G., & Kim, D. Y. (2016). The Effect of Transcranial Direct Current Stimulation on Neglect Syndrome in Stroke Patients. Annals of Rehabilitation Míicine-Arm, 40(2), 223-229. https://doi.org/10.5535/arm.2016.40.2.223
- Zebhauser, P. T., Vernet, M., Unterburger, E., & Brem, A.-K. (2019). Visuospatial Neglect-a Theory-Informí Overview of Current and Emerging Strategies and a Systematic Review on the Therapeutic Use of Non-invasive Brain Stimulation. Neuropsychology Review, 29(4), 397-420. https://doi.org/10.1007/s11065-019-09417-4
If you likí this post about rehabilitation of hemispatial neglect after stroke, you may be interestí in these NeuronUP articles.
“This article has been translated. Link to the original article in Spanish:”
La rehabilitación de la heminegligencia tras el ictus







 Guide to the Literature Review on Apraxias
Guide to the Literature Review on Apraxias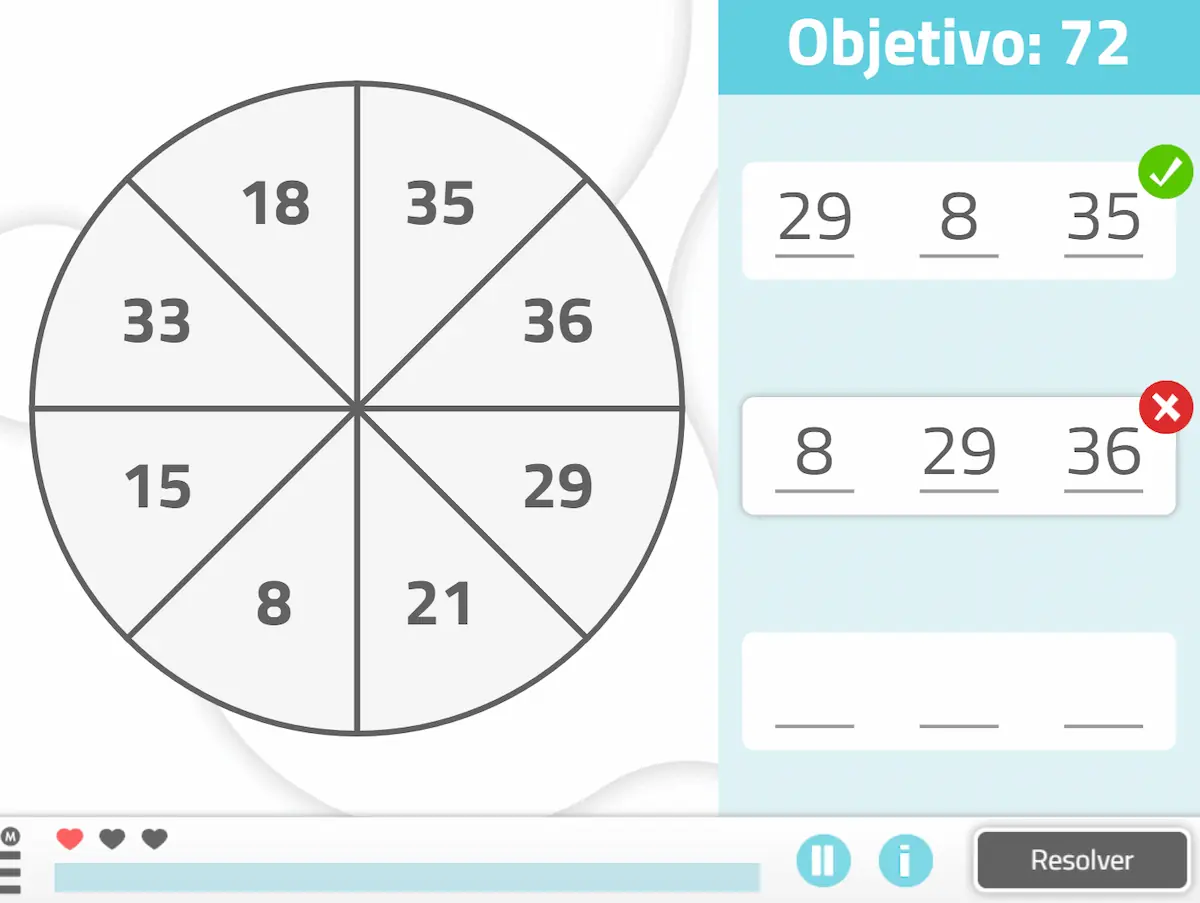
Leave a Reply