Occupational therapist Ángel Sánchez, after explaining in a previous post the objectives and functions of occupational therapy, speaks to us today about the role of occupational therapy in patients with acquired brain injury.
Occupational therapy constitutes the purposeful use of activity or interventions designed to achieve functional goals that promote health, prevent disease and that develop the improvement, maintenance or recovery of the highest possible level of independence for any individual who has suffered an injury, illness or other difficulties, in this case for patients who present acquired brain injury (ABI).
Introduction
The fundamental objective of occupational therapy is to enable the individual to carry out those activities they consider essential in their life. The occupational therapist assesses the underlying motor, cognitive, perceptual and interpersonal skills involved in activities of daily living, as well as occupations and personal roles. Depending on the person’s potential for recovery, they facilitate the performance of activities through improving skills, teaching and developing compensatory and restorative strategies in order to maintain personal independence.
This intervention is characterized by having traits inherent to the professional practice of occupational therapy, to highlight among others:
- Enable the patient with ABI to be independent in their activities of daily living (hereafter, ADLs).
- Establish new roles and meaningful activities for the patient.
- Provide strategies that will facilitate the generalization of learnings from the clinical setting to everyday life.
- Use the analysis, selection and development of activities as a therapeutic intervention process to contribute to achieving the patient’s relevant goals.
The acquired brain injury defines a group of patients who have in common the characteristic of having suffered an event that has interrupted their life development. Within this heterogeneous group of patients, those who have suffered a stroke or a traumatic brain injury are the most frequent, although we can also find those who suffer from brain tumors, assaults, encephalitis and multiple causes of cerebral anoxia (apnea, intoxications, myocardial infarctions, etc.). Traffic, work or sports accidents, increased life expectancy and improved acute care for these patients are factors that contribute to increasing their morbidity.
Main deficits
It is difficult to establish a general pattern of impairment after an ABI, since the alterations found will depend on various factors, among which the initial severity of the injury, its type and location and the presence of complications in the acute phase stand out, not forgetting other relevant factors such as age, personality and cognitive abilities prior to the accident.
Among the main deficits are worth noting the sensory-motor impairments (changes in muscle tone, coordination and motor control, decreased superficial and/or deep sensation); language and communication problems (different forms of aphasia, dysarthria, difficulties in verbal fluency and skills related to communicative pragmatics); and neuropsychological disorders (cognitive and behavioral).
These impairments should not be considered in isolation but with special attention to the difficulties they produce in the patient’s daily functioning when carrying out their ADLs.
Activities of daily living
ADLs are those occupational tasks that a person performs daily according to their biological, emotional, cognitive, social and work role, within which we differentiate:
- Basic ADLs: those that encompass the most basic and necessary self-care capacities such as nutrition, personal hygiene, dressing, bowel and bladder control, mobility and transfers.
- Instrumental ADLs: those that are more complex in nature and require greater elaboration to be carried out and indicate the person’s capacity to lead an independent life in their community. Notable examples are: shopping, handling money, meal preparation, driving, using public transportation, etc.
The fundamental objective of occupational therapy is to enable the individual to develop meaningful activities within their personal roles in the most independent way possible. Traditionally the intervention related to this type of patient has been divided into two models:
- The recovery model, which is based on the restoration of physical, cognitive and perceptual capacities.
- The adaptation or functional model, which emphasizes the use of the capacities that the individual retains in order to compensate for their deficits.
Description of the models
The treatment principle of the recovery model uses activities that require cortical information processing focusing on the stimulation of the affected function in order to produce new neuronal connections and in particular using tasks whose objective is the analysis of the affected capacities for information processing. Implicitly it therefore assumes that the subject will be able, once function is recovered, to generalize this learning to any context and situation.
For its part, the adaptation or functional model is based on the idea that the brain has the capacity to reorganize and also recover its capacity for information processing to some extent; in this way, it helps the person learn to prioritize their residual potential and to use strategies to substitute for or compensate their limitations.
Assessment and treatment
Assessment and treatment are based on functionality (ADLs), that is, on what the patient can or cannot perform. It also emphasizes the individual’s awareness of their situation in relation to their physical, cognitive and perceptual limits so that their treatment can be addressed (internal compensation). Likewise, it recognizes that development will occur if the environment or the task is modified to accommodate the person’s characteristics (external compensation).
It is also important to consider a reflective model of brain injury care where decision-making is conceptualized based on clinical reasoning together with the available scientific evidence to offer perspectives in the approach to the patient so that such decision-making responds to the user’s needs by selecting appropriate therapeutic strategies at each stage of the subject’s evolution through the agreed establishment of the rehabilitation process.
Activity-based intervention
Occupational therapy makes possible learning and recovery through modification of environmental stimuli, in the way occupational tasks are presented and in modification of the context in which they take place. Therefore, it bases its intervention on activity, for the following reasons:
- It is the way to maximize the potential of each patient to improve deficits resulting from the injury, as well as to prevent possible disabilities arising from them.
- Minimizes as much as possible dependency processes by enabling the individual to develop the activities relevant to their personal roles.
- Reduces restrictions in participation by facilitating the acquisition of new roles and addressing the rehabilitation process as holistically as possible, preserving and always taking into account the subject’s likes and preferences whenever possible.
- Stimulates and facilitates the generalization of learning by approaching rehabilitation from the most ecological setting possible, that is, carrying out activities of daily living directly and in a real context. This fact positions occupational therapy as one of the disciplines most appropriate for the treatment of this type of patients since it thus ensures that learning and its implementation are carried out effectively.
Activity and cognitive functions
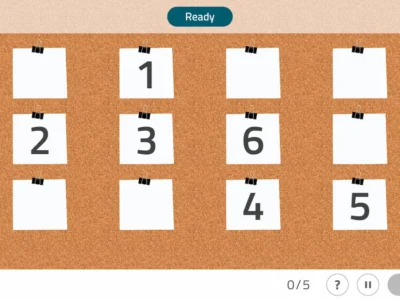
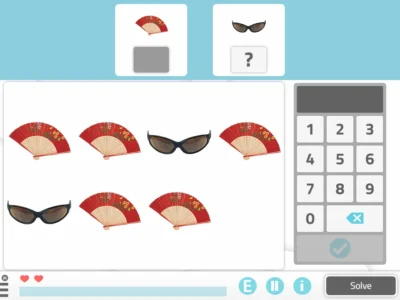
Practice understood as the repetition of isolated movements or cognitive functions tends to decrease in favor of practice opportunities developed in functional activities in different contexts. Occupational therapy uses this knowledge to structure the conditions of professional practice, attempting to focus on determining the necessary conditions during the learning acquisition phase to try to optimize retention and transfer of the learnings acquired by the patient.
Current research indicates that the skills required to complete a “real” activity cannot be acquired in contexts far removed from reality, nor through exclusively repetitive activities.
The occupational therapist modifies the environment to stimulate the motor or cognitive behaviors and strategies they wish to work on for therapeutic purposes. It is worth noting that recent results indicate the efficacy of activity as a therapeutic medium above programs based on isolated, repetitive exercises.
The basic tool of occupational therapy
The basic tool of occupational therapy is activity analysis in which the therapist determines and selects those tasks that will be useful for the therapeutic purposes established based on the patient’s characteristics. Its use will have three general functions:
- Assessment of ADLs
- Tool for assessing skills: motor, cognitive, behavioral, etc.
- Treatment goal
These goals add to the general summary about the understanding of the patient’s global situation in relation to their personal interests, roles and existing capacities after the injury, in order to establish the purposeful activities that will be used as a treatment modality.
Individualized treatment
Referring to the patient’s skills, the occupational therapist assesses ADLs in the context in which they are to be carried out to determine which components are necessary to perform them and compare them with the skills the patient has after the brain injury. This makes possible the development of an individualized treatment plan aimed at remedying and compensating deficits that can be improved, as well as establishing appropriate guidelines for patient management.
This analysis includes, from a sensorimotor perspective, the appropriate “postural set” to carry out a daily activity, as well as the structuring of the cognitive components of the activity and the contextual variables that may influence its performance.
The use of activity in occupational therapy differs from the use of activities by other professionals in:
- It has a dual purpose. On the one hand, completing an activity appropriately from the patient’s point of view, according to their age, gender, environment and interests. On the other hand, improving the deficits the subject presents, stimulating their recovery.
- The ability of the occupational therapist to adapt the selected aspects and contextual conditions of the activity. Thus, adapting the material, form of presentation, size, weight, texture, order, rules and procedures to complete the activity is a basic characteristic of occupational therapy treatment.
- The occupational therapist acts as a facilitation technique to carry out the task. We can perform this function in multiple ways: placing the patient in the correct position before starting, lengthening certain muscle groups that are required actively in the task, through the application of relevant visual or verbal stimuli, guided movements, using orthotic/prosthetic devices, etc. These stimuli are graded in difficulty over time until the patient can successfully meet the task demands without help. Likewise, the occupational therapist plays a fundamental role in the early stages of the patient’s learning to prevent the development of compensatory strategies that could lead to undesirable secondary deficits.
- The selection of the activity is unique for each patient and addresses the person with ABI as unique and different from any other patient with the same pathology.

Subscribe
to our
Newsletter
Purposes of therapeutic occupation
The use of therapeutic occupation is carried out with two purposes:
- Occupation as an end is purposive by definition. The purposive nature of occupation as an end is reflected in its ability to organize people’s behavior, day-to-day life and the lives of individuals. It is not only purposive, but also meaningful. The performance of activities or tasks that a person carries out is related to the importance they attach to them. Only activities that are meaningful to individuals remain in their habitual behavior repertoire.
- Occupation as a means refers to its role as an agent producing therapeutic change to remediate deficits in the individual’s skills or capacities. Occupation in this sense is synonymous with the concept called “purposeful activity.” Purposeful activity demands more specific and particular responses than occupation as an end.
What makes occupation as a means therapeutic?
- The activity must have a purpose or an objective that demands the need for change and allows for achieving success.
- It must have meaning and relevance to the person carrying out that change, which will motivate learning and improvement.
Therefore, the therapeutic aspect of occupation used as a means to change deficits lies in its purposive and meaningful nature.
It is based on the premise that activity itself has therapeutic properties that produce organic changes or improvements in behavioral deficits. However, these inherent aspects are not easily identifiable in the analysis of the activity that takes place during the occupational therapy process.
While meaningful occupation has purpose in itself, strictly speaking, a purposeful activity may or may not be meaningful. The purpose of an activity is the goal, that is, the expected final outcome. Meaning is the value it has for the person and complements the goal. Therefore, it is an individual element that depends on beliefs, preferences, context and culture, as well as the expectations the patient has in their recovery process.
During therapy the meaning develops through personal exchange between the patient and the therapist, to construct and give meaning to activities within a cultural context, moment and life and disability experience taking into account present needs.
Main aims in occupational therapy intervention for patients with acquired brain injury
The following broadly describe some of the main aims in the intervention carried out by occupational therapy in patients with ABI:
Correct postural alignment
The weakness of certain muscle groups and the loss of motor control over the postural adjustments necessary in the limbs and trunk are the main alterations we can observe after an ABI. Therefore the prevention and treatment of musculoskeletal alterations secondary to the injury is achieved through correct postural alignment in the different positions in which the subject carries out their daily activities (supine, sitting, standing); additionally it is necessary to emphasize the importance of correct positioning of the patient in the early phases after brain injury (positioning systems), as well as the necessary practice of different motor tasks.
Assessment and restoration of postural alignment
The patient with brain injury often presents a loss of the ability to effectively associate certain muscle chains to particular actions (for example, using a spoon at mealtime); which could be due to alteration of muscle tone in the structures involved, lack of joint alignment or the loss of the motor engram necessary to carry out a sequence of movements. The role of occupational therapy at this level will basically consist of the appropriate assessment of the affected elements and the restoration of postural alignment and facilitation of the appropriate muscle kinetic chains to successfully complete ADLs.
Stimulating the patient’s metacognition
Occupational therapy must stimulate the patient’s metacognition particularly in the early phases of recovery of the subject’s awareness of their own illness, highlighting the deficits they present so that the subject can anticipate the difficulties they will encounter when facing a particular activity, estimate possible outcomes and evaluate their performance when carrying it out.
Subsequently it will teach the patient general strategies to be practiced in multiple contexts. For example, gathering the relevant information to carry out a task such as preparing a coffee before doing it can serve as a strategy for the patient that stimulates supervision and the establishment of the motor plan to be carried out and the possible difficulties they would encounter during the performance of this activity. We will likewise facilitate their planning and execution.
Cognitive strategies
Just as muscle kinetic chains and postural alignment serve as a basis for correct motor function, the cognitive strategies provide the appropriate frame of reference to stimulate the patient’s ability to interpret and manage complex information coming from different situations and contexts. These strategies aim for the subject to be able to select relevant information from the environment and the activity while discarding what is not relevant and could disrupt correct information processing, in order to plan the most appropriate behavior (motor, sensory, etc.).
Similarly, it cannot be forgotten, especially in acquired brain injury, that performing an ADL always requires the participation and integration of a series of prerequisites or basic components at the sensorimotor, cognitive and behavioral levels whose alteration has a direct relationship with the functional limitations that may occur and their implication in ADL performance.
Needs assessment
It is also the occupational therapist’s role to assess needs related to the recommendation of assistive devices or supportive products that promote the patient’s personal independence, such as long-handled shoehorns to put on shoes or adapted cutting boards for food preparation, among others. Likewise, this professional is responsible for tasks related to home adaptations and accessibility of the places the patient frequents [33]. Finally, the preparation of documents related to professional practice cannot be overlooked, such as administrative documentsrelated to the level of dependency for performing activities of daily living or whether or not there is a need for the use of different assistive products.
The characteristics of the patient with brain injury require a specific approach in terms of assessment and treatment, highlighting the importance of their cognitive deficits as long-term elements predictive of poor functional prognosis in relation to the need for third-party help to perform ADLs.
Generalization
The objective of Occupational Therapy for the patient with ABI should focus on the generalization of new skills carried out in multiple real contexts.
It is recommended to use ADLs as both an end and a therapeutic means, rather than practicing isolated exercises repetitively, taking into account the patient’s characteristics after the injury.
Occupational Therapy as a discipline has acquired in the last decade an increasingly relevant role both in hospital treatment and in the community context, showing its effectiveness, cost-effectiveness and necessity for improving functional outcomes in patients who have suffered acquired brain injury.
Bibliography
- García Peña M, Sánchez Cabeza A, Miján de Castro E. Evaluación funcional y terapia ocupacional en el daño cerebral adquirido. Rehabilitación (Madr) 2002; 36 (3): 167-75.
- Hinojosa J, Sabari J, Pedretti L. Position paper: purposeful activity. Am J Occup Ther 1993; 47: 1081-85.
- Jackson JD. After rehabilitation: meeting the long-term needs of persons with traumatic brain injury. Am J Occup Ther 1994; 48: 251-255.
- Tickle-Degnen L., Rosenthal R. The behavioural and cognitive response of brain damaged patients to therapist instructional style. Occupl Ther J Res 1990; 10: 345-59.
- Mathiowetz V, Bass Haugen J. Motor behaviour research: implications for therapeutic approaches to central nervous system dysfunction. Am J Occup Ther 1994; 48: 733-39.
- Ministerio de Trabajo y Asuntos Sociales. Secretaría de Estado de Servicios Sociales. Familias y Discapacidad. Instituto de Mayores y Servicios Sociales (IMSERSO) (2001). Organización Mundial de la Salud Clasificación Internacional del Funcionamiento, de la Discapacidad y de la Salud (CIF). Madrid: IMSERSO;2001.
- Mulder T. A process-oriented model of human motor behaviour: toward a theory based rehabilitation approach. Phys Ther 1991; 71: 157-63.
- Nashner LM, McCollum G. The organization of human postural movements: a formal basis and experimental synthesis. Behav Brain Sci 1985; 8: 135-39.
- Neistadt ME. Occupational therapy for adults with perceptual deficits. Am J Occup Ther 1988; 42: 434-40.
- Toglia JP. Approaches to cognitive assessment of the brain injured adult: Tradicional methods and dynamic investigation. Occup Ther Prac 1989; 1: 36-55.
More bibliography
- Bakshi R, Bhambhani Y, Madill H. The effects of task preference on performance during purposeful and nonpurposeful activities. Am J Occup Ther 1991; 45: 912-16.
- Jarus T. Motor learning and occupational therapy: the organization of practice. Am J Occup Ther 1994;48: 810-14.
- Higgins JR, Spaeth RK. Relationship between consistency of movement and environmental condition. Quest 1972; 17: 61-67.
- Sabari JS. Motor learning concepts applied to activity-based intervention with adults with hemiplegia. Am J Occupl Ther 1991; 45: 523-26.
- Shumway-Cook A, Woollacott M. Motor control: theory and practical applications. Baltimore: Williams and Wilkins; 1995.
- Schimidt RA. Motor learning principles for physical therapy. En: Lister MJ, editor. Contemporary management of motor control problems: proceeding of the II Step conference. Alexandria: Foundation for Physical Therapy; 1991. p.1-20.
- Trombly C.. Clinical practice guidelines for post-stroke rehabilitation and occupational therapy practice. Am J Occup Ther 1995; 49:711-715
- Trombly CA. Occupation: purposefulness and meaningfulness as therapeutic mechanisms. Am J Occup Ther 1995; 49: 960-63.
- Winstein CJ. Designing practice for motor learning: clinical implications. En: Lister MJ, editor. Contemporary management of motor control problems: proceeding of the II Step conference. Alexandria: Foundation for Physical Therapy; 1991. p.65-76.
- Zimmerer-Branum S, Nelson DL. Occupationally embedded exercise versus rote exercise: a choice between occupational forms by elderly nursing home residents. Am J Occup Ther 1995; 49: 397-41.
More references
- Abreu BC. The effect of environmental regulations on postural control after stroke. Am J Occup Ther 1995; 49: 517-25.
- Abreu BC. The quadraphonic approach: Management of cognitive-perceptual and postural control dysfunction. Occup Ther Prac. 1992; 3: 12-29.
- Carr JH, Shepherd RB. A motor relearning program for stroke Ed 2º. Rockville, Md: Aspen; 1987.
- Carr JH, Shepherd RB. Early care of the stroke patient: a practice approach. London: Heinemann; 1983.
- Davies PM. Steps to follow. A guide to the treatment of adult hemiplegia. New York: Springer-Verlag; 1985.
- Magill RA. Motor learning concepts and applications. 4th ed. Madison: Brown and Benchmark; 1993.
- McCoy AO, Van Sant AF. Movement patterns of adolescent rising from a bed. Phys Ther 1993; 73:182-86.
- Morton GG, Barnett DW, Hale LS. A comparison of performance measures of an added-purpose task versus a single-purpose task for upper extremities. Am J Occup Ther 1992; 46: 128-32.
- Neistadt ME. The neurobiology of learning: Implications for treatment of adults with brain injury. Am J Occup Ther 1994; 48: 421-30.
- Toglia JT. Generalization of treatment: a multicontext approach to cognitive perceptual impairment in adults with brain injury. Am J Occup Ther 1991; 45: 505-09.
- Toglia JP. Visual Perception of objects: an approach to assessment and intervention. Am J Occup Ther 1989; 43: 587-94.
- Radomski MV. Occupational therapy practice guidelines for adults with traumatic brain injury. USA: American Occupational Therapy Association; 1997.
- Sánchez-Cabeza A, García-Peña M. Reflexiones sobre el proceso de tratamiento de las disfunciones cognitivas y perceptivas. Revista informativa de la Asociación Profesional Española de Terapeutas Ocupacionales 2002; 28: 2-13.
If you liked this article by occupational therapist Ángel Sánchez about occupational therapy in patients with acquired brain injury, you might also be interested in the following articles:
“This article has been translated. Link to the original article in Spanish:”
Terapia ocupacional en pacientes con daño cerebral sobrevenido





 Ana Belén Vintimilla answers questions about her lecture on neurodevelopment in pediatric brain injury
Ana Belén Vintimilla answers questions about her lecture on neurodevelopment in pediatric brain injury
Leave a Reply