The specialist in child neuropsychology José Oré delves into neurodevelopment, the classification of neurodevelopmental disorders, their comorbid presentations and their neuropsychological assessment.
Currently there is an increase in emotional and behavioral disturbances in childhood and adolescence in Peru (Instituto Nacional de Salud Mental Honorio Delgado- Hideyo Noguchi), which can be described and explained depending on their etiology, symptomatology and dysfunctionality in child and adolescent disorders, among which are the neurodevelopmental disorders.
The child and adolescent disorders have different etiologies from a biological, psychological and social perspective. One of those large groups is made up of neurodevelopmental disorders.
This group of disorders is characterized by a delay in brain growth and maturation associated with cognitive, emotional, behavioral dysfunction (Artigas- Pallarés, Guitart & Gabau- Vila, 2013).
Below, we will describe the construct of neurodevelopment, the classification of neurodevelopmental disorders, their comorbid presentations and their assessment from a neuropsychological perspective.
Neurodevelopment
Neurodevelopment involves a constant interaction between the organism and the environment, in which different capacities, abilities, skills, attitudes, etc. are progressively formed, in which the nervous system enters a process of maturation and together with the social environment allows the development of brain functions, as well as personality (Gutiérrez, Lazarte & Alarcón, 2016).
In addition, it allows the maturation of cognitive, motor and emotional capacities, although it starts from a similar process, each person has their own pace, being a link for an adequate interaction of genetics, stimulation and affection (Medina-Alva, et al., 2015).
Consequently, its delay can give rise to a reduced connection and development of the brain, described through neurodevelopmental disorders.
What are neurodevelopmental disorders?
Neurodevelopmental disorders are problems associated with reduced functioning and performance of the nervous system that begin in early childhood and usually manifest as motor disturbances, behavioral problems, difficulties in social interaction, language and learning (Galán-López, Lascarez-Martínez, Gómez-Tello & Galicia-Alvarado, 2017).
Classification of neurodevelopmental disorders
Montes, Bembibre, Triviño and Arnedo (2015) classify neurodevelopmental disorders as genetic, of environmental etiology and those defined by their final repercussions. To the extent that abnormal warning signs and risk factors are identified at the prenatal, perinatal or postnatal level, their evolution and/or prognosis can be known (Ponce-Meza, 2017).
The most common genetic disorders are Down syndrome, Edwards syndrome, Klinefelter syndrome, etc.; among the disorders of environmental etiology are those derived from drug use, malnutrition, parasitic or bacterial infections; and the disorders of functional repercussion include attention deficit hyperactivity disorder, autism spectrum disorder, language disorder, learning disorders and intellectual disability.
Depending on their diverse etiology, detection is convenient in order to subsequently provide strategies that stimulate their capacities and their altered circuits for a greater potential for development (Artigas-Pallarés, Guitart, Gabau-Villa, 2013).
They can be approached from a neurological, psychiatric and psychological perspective. One of the specialties of psychology that is responsible for the detection, assessment, diagnosis and intervention of delays and/or neurodevelopmental disorders is child neuropsychology (Arango- Lasprilla, Rivera y Olabarrieta- Landa, 2017).

Subscribe
to our
Newsletter
Child neuropsychology
Child neuropsychology is a behavioral neuroscience that studies the relationships between behavior and the developing brain (Cuervo & Ávila, 2010).
This specialty is responsible, from a neuropsychological approach, for neurodevelopmental disorders such as attention deficit hyperactivity disorder, ADHD, autism spectrum disorders, ASD, congenital malformations, congenital disorders and learning difficulties (Montes, Bembibre, Triviño & Arnedo, 2015).
The theoretical framework of child neuropsychology consists of the relationship that the child’s brain has with its environment, in which the different brain areas and cognitive functions are in constant maturation, thus allowing greater functionality and adaptation to respond to different situations they may face.
Meanwhile, if there were a neurocognitive delay, brain plasticity will allow compensating for and restoring these deficiencies (Arango- Lasprilla, Romero, Hewitt- Ramirez y Rodriguez, 2018).
Role of the child neuropsychologist
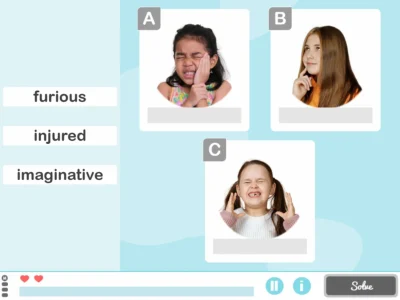
One of the roles of the child neuropsychologist is the neuropsychological assessment, that is, the use of techniques and instruments to evaluate the development of cognitive, emotional and behavioral functions resulting from the functioning of the developing nervous system (Portellano & García, 2014).
This helps contribute to the differential diagnosis of different child and adolescent conditions such as neurodevelopmental disorders, externalizing disorders, internalizing disorders, etc. (Arango- Lasprilla, Rivera, & Olabarrieta-Landa, 2017).
From a practical description, a parents’ press conference is held to collect the reason for consultation and the neuropsychological clinical history, the cognitive areas are explored with neuropsychological instruments and it is observed how the child responds to the tasks (stimuli) presented and whether they are congruent with their chronological age (Oré, 2019).
Neurodevelopmental disorders and comorbidity
Most neurodevelopmental disorders do not manifest independently with a similar course, main symptoms or a specific age of onset, so their diagnosis is confusing or incomplete; within clinical practice they mostly present as comorbid or associated conditions.
Comorbidity, therefore, consists of the occurrence in the same person of two or more pathologies, where the onset of one determines its prognosis and intervention process (Montes, Bembibre, Triviño y Arnedo, 2015).
The disorders with the greatest comorbidity correspond to ADHD and ASD. Although each of these disorders have main symptoms that distinguish them from others, it is advisable to explore other conditions that may be associated (Arango- Lasprilla, Romero, Hewitt- Ramírez & Rodríguez, 2018).
ADHD
ADHD is a neurodevelopmental disorder that is characterized by a persistent pattern of inattention, hyperactivity and impulsivity (American Psychiatric Association, 2015).
Below, we detail its 3 predominance types: Predominantly inattentive, hyperactive and combined (inattention, hyperactivity and impulsivity). Also, its main comorbidities are Learning disorders (LD), Conduct disorders (CD) and Anxiety disorders (AD).
Subtypes and comorbidities
Predominantly inattentive ADHD is often associated with Learning Disorders (LD), commonly with reading and writing problems (Scandar, 2013). It should be noted that both problems fall under the category of neurodevelopmental disorders.
Therefore, a deficit in attentional functions would generate difficulties in learning areas such as reading, writing, spelling. Mostly, this is observed in girls compared to boys in a clinical setting.
Predominantly hyperactive-impulsive and combined ADHD, that is, with greater hyperactivity and impulsivity symptomatology, tends to be associated with or differentiated from other behavioral disturbances also called externalizing disorders such as Oppositional Defiant Disorder (ODD) or conduct disorder (CD) (Baca, 2012).
Differences with other disorders
One of the main differences stems from the etiology of the problem; mostly children with ADHD have problems in their development process where they show cognitive and emotional immaturity, whereas ODD and CD usually arise from a harmful and inadequate environment that reinforces their maladaptive behaviors causing children not to respect social norms.
Similarly, depending on the evolution of the problem, while in children with ADHD symptoms are expected to decrease in adolescence, in ODD maladaptive problems may increase, possibly progressing to CD.
If the symptoms of these disorders begin at a younger age, the prognosis tends to be unfavorable (Arango- Lasprilla, Romero, Hewitt- Ramirez y Rodriguez, 2018).
Likewise, another relationship is usually noticeable with mood disorders, specifically with a higher frequency of anxiety disorders and to a lesser extent depressive disorders.
This would imply that the child with ADHD may feel down, worried, tense, pessimistic and guilty because they cannot perform academically or socially like other children in their environment.
These symptoms and even more so their differences are difficult to determine because their social environment such as family, teachers and peer groups would be more attentive to their hyperactivity and attention problems.
For this reason, it is recommended to find out if there are family members with a history of emotional problems. It is also important to know if the main ADHD symptoms have generated depressive and/or anxious symptomatology (López-Villalobos, Serrano & Sánchez-Mateos, 2013).
ASD
ASD is a neurodevelopmental disorder whose deficits focus on communication and social interaction as well as restrictive and repetitive patterns of behaviors, interests and activities (American Psychiatric Association, APA, 2015).
Next, we delve into its main comorbidities such as epilepsy, ADHD, intellectual disability (ID), sleep disorders, anxiety disorders, aggression and a deficit in social skills.
Comorbidities
Epilepsy has a large neuropsychological component, so it is important to detect early cognitive deficits and differentiate them from other conditions (Arango- Lasprilla, Romero, Hewitt- Ramírez & Rodríguez, 2018).
Mostly in ASD and epilepsy there are cases of intellectual disability, as well as language, declarative memory and executive function impairments, which would result in a worse prognosis for the child’s development and functionality (García-Peñas, 2009).
Between 20% and 30% of children with ADHD may present ASD (Rico-Moreno & Tárraga- Mínguez, 2016). The comorbidity of both conditions could be explained by an alteration in the development of executive functions.
In fact, in both disorders it is observed that children show a maturational delay in executive functioning of inhibitory control, cognitive flexibility and planning.
A differentiation in executive performance would include that ASD present greater difficulties in cognitive flexibility and abstraction, however, in ADHD the executive deficit would correspond to inhibitory control and working memory (Portellano y García, 2014).
Regarding ID and ASD we can indicate similarities in the alterations associated with intellectual performance. Mostly in both disorders an below-average intellectual quotient is observed, as well as difficulties in social maturity, due to poor adaptation to change and decreased cognitive flexibility, except in cases of high-functioning ASD such as Asperger Syndrome where intellectual performance stands out compared to other children (Montes, Bembibre, Triviño y Arnedo, 2015).
Finally, sleep disorders, anxiety disorders and aggression would be secondary disturbances within ASD.
Moreover, depending on the possible etiology and comorbidity, insomnia, night terrors, tension, fear, worry and even impulsive reactions that break social norms could be observed (Arango- Lasprilla, Romero, Hewitt- Ramirez y Rodriguez, 2018).
The importance of neuropsychological assessment
Therefore, it is of great importance to carry out a neuropsychological assessment in the different disorders or alterations of neurodevelopment, since it makes it possible to detect cognitive performance, whether in strengths, weaknesses or average performance.
These results together with the psychopathological examination generate a better analysis to detect the onset, evolution and prognosis of the problem which would lead to an appropriate diagnosis and therefore a good start of neuropsychological, psychological, neurological or psychiatric intervention considering its comorbidity in each case (Pardos, 2019).
Conclusions
The article allows understanding the characteristics of neurodevelopmental disorders, one of the main manifestations being the delay in brain growth and/or maturation, which as a consequence brings cognitive, emotional, behavioral and social dysfunction in the child and adolescent.
Likewise, their classification based on genetic disorders, disorders of environmental etiology and disorders defined by their final repercussions was described.
Specifically in this latter group are attention deficit hyperactivity disorder, autism spectrum disorder, language disorder, learning disorders and intellectual disability.
Meanwhile, one of the disciplines that studies them from a clinical perspective is child neuropsychology, whether carrying out activities of detection, assessment and intervention of the brain-behavior relationship in neurodevelopmental disorders.
On the other hand, most neurodevelopmental disorders show comorbid conditions, the most comorbid being attention deficit hyperactivity disorder and autism spectrum disorder, however, there are other conditions that also need to be detected, described and differentiated to have a better analysis of their prognosis, diagnosis and intervention, with neuropsychological assessment being one of the procedures of great importance.
Bibliography
- Arango- Lasprilla, J. ; Romero, I. Hewitt- Ramirez, N. & Rodriguez, W. (2018). Trastornos psicologicos y neuropsicologicos. Bogotá, Colombia: Manual Moderno.
- Arango- Lasprilla, J., Rivera, D. & Olabarrieta- Landa, L. (2017). Neuropsicología infantil. México D.F: Manual Moderno.
- Arnedo, M., Montes, A., Bembibre, J, & Triviño, M. (2015). Neuropsicología infantil a través de casos clínicos. España: Médica Panamericana.
- Artigas- Pallarés, J., Guitart, M. & Gabau- Vila, E. (2013). Genetic bases of neurodevelopmental disorders. Revista Neurol, 56, (1), 23-34.
- Asociación Americana de Psiquiatría (2015). Manual diagnóstico y estadístico de los trastornos mentales. España: Editorial Medica Panamericana.
- Baca, F. (2012). Trastornos del inicio del comportamiento disruptivo en estudiantes de 8 a 11 años de una institución educativa del Callao (Unpublished master's thesis). Universidad San Ignacio de Loyola, Lima. Recuperado de: repositorio.usil.edu.pe/
- Cuervo, A., & Ávila, A. (2010). Developmental child neuropsychology: Detection and intervention of disorders in childhood. Revista Iberoamericana de Psicología: Ciencia y Tecnología, 3(2), 59-68.
- Galán-López, I., Lascarez-Martinez, S., Gómez-Tello, M. & Galicia-Alvarado, M. (2017). Comprehensive approach to neurodevelopmental disorders. Revista del Hospital Juárez de México, 84(1), 19-25.
- García-Peñas (2009). Autism, epilepsy and pathology of the temporal lobe. Revista de Neurología, 48(2), 35-45.
- Gutiérrez, E., Lazarte, F. & Alarcón, G. (2016). The importance of the evaluation of neurodevelopment in children under thirty months in the Peruvian context. Acta Médica Peruana, 33(4), 304-308.
If you enjoyed this post about neurodevelopment: disorders, comorbidity and child neuropsychology, you might also be interested in:
“This article has been translated. Link to the original article in Spanish:”
El neurodesarrollo: trastornos, comorbilidad y neuropsicología infantil





 Neurorrehabilitation or neurorehabilitation: How is it written?
Neurorrehabilitation or neurorehabilitation: How is it written?
Leave a Reply