The occupational therapist at the AFA Alcalá center, Laura Caballero, explains the approach to neurodegenerative diseases through cognitive stimulation workshops and occupational therapy using NeuronUP.
Introduction
Who are we?
The Association of Relatives and Patients of Alzheimer’s and Parkinson’s of Alcalá de Henares (AFA Alcalá) was founded in 1997 as a resource created by and for the relatives of people with Alzheimer’s disease in order to support each other and achieve a better quality of life for the patient and their families. We are a regional NGO and our members are mostly relatives of people with age-related neurodegenerative diseases such as Parkinson’s, Alzheimer’s and other related dementias.
Our center, where the activities take place, is located in Alcalá de Henares, which is the largest city in the area, but it serves people from neighboring towns.
Interdisciplinary team
Our team is made up of professionals specialized in various areas, such as:
- Psychology
- Occupational therapy
- Art therapy
- Music therapy
- Speech therapy
- Physiotherapy
- Social work
From a transdisciplinary approach we achieve a holistic care for both the person with the disease and their family and social environment.
Neurodegenerative diseases we work with
Below, we briefly detail the various pathologies we receive at our center:
Parkinson
Neurodegenerative, chronic and progressive disease characterized by extrapyramidal symptoms, due to irreversible damage to the substantia nigra that produces dopamine. The symptoms of Parkinson’s disease are:
- Bradykinesia: slowness of voluntary movements associated with a decrease in voluntary movements, with loss of automatic movements, hypophonic speech, absence of arm swing.
- Resting tremor.
- Postural instability: loss of reflexes, stooped gait, increased base of support, gait disorders.
- Rigidity.
In addition to these four core symptoms for the diagnosis of Parkinson’s disease, there are neuropsychiatric alterations such as cognitive impairment, mood disorders, sleep disorders, delusions and hallucinations, bradypsychia, problems with chewing, speaking and food intake. And vegetative symptoms (constipation, incontinence, sweating, salivation, among others.)
Cognitive impairment
Cognitive impairment is the loss of cognitive functions, specifically in memory, attention and information processing speed (IPS), that occurs with normal aging.
This cognitive decline of our brain depends on both physiological and environmental factors and is subject to a great interindividual variability.
The difference between cognitive impairment and dementia must be taken into account. When a person is not independent to cover their basic needs it is considered dementia, but it is true that a person may report certain memory losses or other cognitive functions and still remain independent in everyday tasks; it is then called Mild Cognitive Impairment (MCI).
Several studies have shown that people with MCI are at risk of developing dementia in the future. Cognitive impairment is classified as mild, moderate, severe and very severe; from moderate it begins to be considered dementia.
Dementia
Dementia is a condition associated with age; as the population ages the frequency of the disease increases. Dementia is not a specific disease, it is a general term that describes a wide variety of symptoms related to the deterioration of memory and other cognitive abilities, severe enough to interfere with the activities of daily living of the person.
There are various types of dementia, but only Alzheimer’s, Lewy body dementia and frontotemporal dementia will be described here.
Alzheimer’s disease
It is a progressive neurodegenerative disease characterized by degeneration of the brain’s nerve cells and manifests with memory loss. Initially, short-term memory is lost, and finally long-term memory. It also presents with aphasia, apraxia and agnosia, as well as disorientation in time, space and person, and intellectual deterioration. The deficits are sufficient to interfere with social and occupational functioning, representing a decline from previous function.
Lewy body dementia
People who suffer from dementia with diffuse Lewy bodies have abnormal protein deposits in areas related to cognition. It manifests as dementia, fluctuating cognition and alertness, visual hallucinations that appear from the onset of the disease and are very well formed, motor signs of parkinsonism, rigidity, slowness of movement, and to a lesser extent tremor.
Frontotemporal dementia
A progressive disease characterized by prominent behavioral alterations and changes in language. For example, primary aphasia, difficulty naming, etc. It is also characterized by a series of physical signs such as: incontinence, rigidity, akinesia, tremor, frontal reflexes (glabellar, sucking, palmomental) and behavioral, social, judgment and language deficits disproportionate to memory impairment.
Inclusion protocol: How is the approach to neurodegenerative diseases carried out in the center?
Interdisciplinary assessment
The entry point to our association is through the social work department, where, through a guided intake interview, the most urgent needs are assessed. This first contact serves to confirm whether we are the appropriate resource or, unfortunately, on some occasions we act as intermediaries to other services or institutions.
The next step toward inclusion in workshops is the assessment by the transdisciplinary team. The global assessment at the functional, cognitive and physical level gives us an approximate idea of the state of the disease, as well as the impact it has on the person’s close environment.
Intervention proposal and family guidance
Each professional on the team presents the results of that assessment in a weekly meeting. All this information serves to offer the intervention plan that best fits the needs; everything is taken into account: life history, personality and preferences, family support network, income, level of education, meaningful activities and leisure time.
In family guidance, the center’s psychologist talks about the disease and its progression, management of possible behavioral alterations, questions that may arise and finally offers the proposal designed for their relative.
Inclusion in workshops: cognitive stimulation and occupational therapy in the approach to neurodegenerative diseases with NeuronUP
Once the proposal is accepted by the family, the person is incorporated into a stimulation group with similar cognitive impairment. It is in these workshops that we work on different affected cognitive areas, using different approaches and resources.
From the most conventional and functional tools for them such as pencil and paper to the application of new technologies and resources like the tablet and NeuronUP.
We also resort to other non-pharmacological therapies such as expressive therapies. Specifically music therapy, drama therapy and art therapy, integrated into the day-to-day life of the association.
What is addressed in the approach to neurodegenerative diseases with NeuronUP?

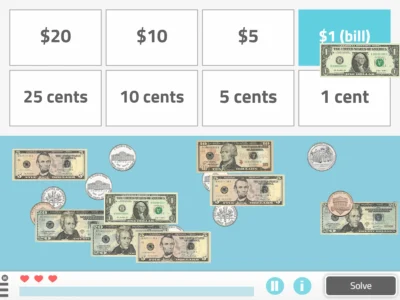
Activities of daily living
As occupational therapists, working in an outpatient setting, it has always been very difficult for us to reproduce in the therapy room those activities of daily living and their therapeutic approach in order to retrain the user in lost skills. It is through NeuronUP that we are able to create a virtual environment to reproduce activities such as dressing, grooming, tidying the kitchen, recycling, sequencing steps, etc.
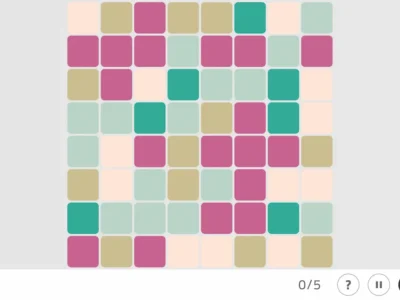
Severe impairment
When the level of deterioration and loss of capacities is very advanced, conventional resources are not sufficient. Therapists resort to different, more sensory resources as a way to reach an optimal level of stimulation for the person. In this respect NeuronUP provides us with auditory and visual resources (movement, color, shape, low speed) adapted to low residual capacities.
Low literacy level
Although stimulation is done in groups, personal prior characteristics such as level of schooling are taken into account. In cases where the person is illiterate or attended school for only a few years, NeuronUP becomes a very valuable resource to adapt stimulation as much as possible.
The use of the application allows us to promote the person’s autonomy during the execution of the exercise, as well as encourage individualized attention.
The visual support (through pictograms and different images) and auditory support (each exercise is explained verbally) in most exercises makes it intuitive to use.
Language impairment
We positively value the large number of resources related to this area that NeuronUP offers. It enables us to work on the same domain through different activities, making the approach motivating by avoiding repetition.
Impulse control
Perhaps this is one of the areas on which we have focused most in recent years. We observe the course of the diseases and how the symptomatology is changing, currently receiving numerous diagnosed people in whom this lack of impulse control makes their daily life difficult.
The dynamics of the exercises themselves allow us to work simultaneously on the affected areas as well as different associated behavioral alterations, such as, inhibition, social cognition, etc.
Conclusion
To conclude, we can say that the therapists who run the center’s cognitive stimulation workshops for addressing neurodegenerative diseases have found NeuronUP to be a fundamental resource that helps us save time, provides a wide range of resources and also allows us to reach a wider range of users.
If you liked this post about the approach to neurodegenerative diseases with NeuronUP, we recommend you take a look at these posts:
“This article has been translated. Link to the original article in Spanish:”
El abordaje de las enfermedades neurodegenerativas con NeuronUP




 Activity to work on emotions with children: What are they feeling?
Activity to work on emotions with children: What are they feeling?
Leave a Reply