Mental illnesses or mental health disorders represent one of the greatest public health challenges worldwide. In recent decades, the approach to their treatment has evolved significantly thanks to advances in scientific research and the integration of new technologies. This article explores the most notable trends in the treatment of mental illnesses, focusing on innovative strategies, emerging technologies and multidisciplinary approaches.
What are mental illnesses?
Mental illnesses are disorders that affect a person’s thinking, emotions, behavior and social interactions, directly interfering with their ability to maintain quality of life.
These conditions encompass a wide range of diagnoses such as depression, anxiety, bipolar disorder, schizophrenia and eating disorders.
What is bipolar disorder?
The bipolar disorder is a mental illness characterized by extreme mood fluctuations, ranging from manic or hypomanic episodes (a feeling of euphoria or hyperactivity) to depressive episodes.
There are two main types of bipolar disorder:
- Bipolar I: It is characterized by severe manic episodes followed by significant depressive episodes. These last at least one week, although they may require hospitalization for the affected person.
- Bipolar II: Involves hypomanic episodes (less severe than mania) together with severe depressive episodes.
What is schizophrenia?
The schizophrenia is a chronic mental disorder characterized by psychotic symptoms such as hallucinations, delusions, disorganized speech and thought disorders; as well as low motivation and reduced expressivity; in addition to cognitive deficits involving impairment of executive functions, memory and processing speed. This conjunction of diverse symptoms can make communication and interpersonal relationships difficult for those who suffer from it.
Although schizophrenia is less common than bipolar disorder, its effects on quality of life are profound, with symptoms that require constant intervention and a multidisciplinary approach to treatment.
What are the risk factors for mental illnesses?
Mental illnesses such as bipolar disorder and schizophrenia have a strong genetic basis. However, they are also influenced by environmental and biological factors.
- Genetic factors: Research has shown that having a family history of psychiatric disorders significantly increases the risk of developing these types of mental illnesses.
- Biological factors: Imbalances in neurotransmitters such as dopamine and serotonin, as well as alterations in brain structure, are key components in conditions like bipolar disorder and schizophrenia.
- Environmental factors: Variables such as prolonged stress, trauma and traumatic experiences, and substance abuse can trigger or worsen the symptoms of both mental illnesses.

Subscribe
to our
Newsletter
Key trends in the treatment of mental illnesses
As research in neuroscience and psychology advances, treatment strategies for mental illnesses such as bipolar disorder and schizophrenia are also changing. Below, we explore the main trends shaping the treatment of these mental health disorders.
1. Psychosocial therapies and psychoeducation
Psychosocial therapies play a fundamental role in the treatment of bipolar disorder and schizophrenia. With the mission of educating both affected individuals and their families about the illnesses and treatment approaches, psychoeducation is one of the most recent approaches in the therapeutic intervention for these disorders.
Cognitive-behavioral therapy (CBT)
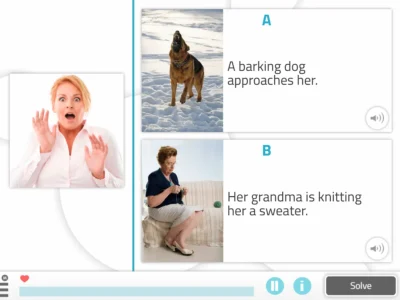
Cognitive-behavioral therapy (CBT) is a psychotherapeutic approach that focuses on identifying and changing negative thought and behavior patterns. This type of therapy is aimed at helping affected individuals identify and modify their negative thought patterns and develop skills to cope with stressful situations.
It is based on techniques of cognitive restructuring and behavior modification, with the aim of promoting long-term psychological well-being.
Cognitive-behavioral therapy (CBT) has been used for years in the treatment of mental disorders, and its effectiveness in bipolar disorder and schizophrenia continues to show promise.
Benefits of psychosocial therapies and psychoeducation in the treatment of mental illnesses
- Improved illness coping: People affected by these mental health disorders learn to better manage manic, depressive or psychotic episodes.
- Reduction of relapses: Psychoeducation helps patients and their families recognize early signs of a relapse and intervene quickly.
2. Noninvasive brain stimulation therapies
Noninvasive brain stimulation has become one of the most promising therapies for the treatment of mental illnesses such as bipolar disorder and schizophrenia. Techniques such as transcranial magnetic stimulation (TMS) and deep brain stimulation (DBS) are being evaluated for their efficacy in treating these disorders.
Transcranial magnetic stimulation (TMS)
Transcranial magnetic stimulation (TMS) is a noninvasive technique that involves using magnetic pulses to stimulate specific areas of the brain with the goal of treating the symptoms of mental illnesses such as depression and bipolar disorder. Recent research has also shown that this type of stimulation can be effective in patients with treatment-resistant bipolar depression.
Its ability to influence brain plasticity makes it an innovative and promising tool in the field of cognitive stimulation and mental rehabilitation.
Deep brain stimulation (DBS)
Deep brain stimulation (DBS) is a surgical treatment that involves implanting electrodes in the brain to regulate abnormal brain signals with electrical impulses to specific areas.
Although it is commonly used in the treatment of other disorders affecting cognition such as Parkinson’s, it is beginning to show positive results in the treatment of psychiatric disorders, especially in treatment-resistant schizophrenia.
This innovative approach to neurorehabilitation can be an option when other treatments are not effective.
Benefits of noninvasive brain stimulation therapies in the treatment of mental illnesses
- Noninvasive treatments: These techniques do not require major surgery and have limited side effects.
- Improved response to conventional treatments: Brain stimulation can improve the response to medication and reduce symptoms.
3. Rehabilitation and cognitive stimulation
Rehabilitation and cognitive stimulation are emerging as key treatments, especially in patients with bipolar disorder and schizophrenia, who often suffer from cognitive impairment.
Through exercises and activities specifically designed to exercise the brain and improve cognitive skills that may be affected, such as memory, attention, problem solving and decision making, rehabilitation and cognitive stimulation is especially useful for patients with schizophrenia, who often exhibit lasting cognitive difficulties.
Rehabilitation and cognitive stimulation provide additional and complementary options to pharmacological treatments and traditional therapies, especially for patients with significant cognitive deficits.
Benefits of rehabilitation and cognitive stimulation in the treatment of mental illnesses
- Reduction of symptom impact, improving the ability to think clearly, make decisions and, ultimately, the overall quality of life of affected individuals.
- Reduction of cognitive dysfunction in people with schizophrenia, thus mitigating the cognitive decline associated with this mental illness.
4. Multidisciplinary approaches
Adopting multidisciplinary approaches in the treatment of mental illnesses such as bipolar disorder and schizophrenia is now considered the standard. Active collaboration among professionals such as psychiatrists, psychologists, occupational therapists and social workers allows for the joint design of a comprehensive intervention for people affected by these mental health disorders.
Benefits of multidisciplinary approach therapies in the treatment of mental illnesses
- Improved treatment adherence and effectiveness, thanks to the collaboration of different disciplines to improve therapeutic outcomes.
- Treatment of associated comorbidities such as anxiety or substance abuse, which also promotes the social reintegration of these people, improving their long-term quality of life.
Conclusion
The treatment of mental illnesses such as bipolar disorder and schizophrenia has advanced significantly in recent years thanks to innovations and advances in psychosocial therapies and psychoeducation, noninvasive brain stimulation therapies, cognitive rehabilitation and the adoption of multidisciplinary approaches, which, when combined effectively, can greatly improve the quality of life of people affected by these mental health disorders. Staying up to date with these trends is crucial for neurorehabilitation professionals seeking to offer effective, evidence-based interventions.
If you enjoyed this blog post about the current trends in the treatment of mental illnesses, you will likely be interested in these NeuronUP articles:
“This article has been translated. Link to the original article in Spanish:”
Tendencias actuales en el tratamiento de enfermedades mentales






 Why use NeuronUP2GO?
Why use NeuronUP2GO?
Leave a Reply