On the occasion of World Schizophrenia Day, Doctor of Psychology Rafael A. Salas Muriel presents in this article, from a neuropsychological perspective, what schizophrenia is, its symptoms, types and how clinical neuropsychology and neuropsychological rehabilitation can contribute to the treatment of this clinical condition, as well as improve the quality of life of those who suffer from it.
What is schizophrenia?
Schizophrenia is a mental disorder that is often chronic and severe, affecting millions of people worldwide. It is characterized by a combination of psychotic symptoms, such as hallucinations and delusions, along with cognitive dysfunctions and problems in social functioning. This disorder can cause significant impairment in the person’s ability to function well in daily life, as well as for the family members and close associates who surround the individual.
One of the most prominent aspects of schizophrenia is the psychotic symptoms, which can include visual or auditory hallucinations (American Psychiatric Association, 2022), in which the person perceives stimuli that do not exist in reality, and delusions, which are false or irrational beliefs that persist despite contrary evidence. These symptoms can be very disabling and confusing, both for the person experiencing them and for their environment.
In addition to psychotic symptoms, schizophrenia is also associated with a range of cognitive dysfunctions, such as memory impairment, attention disturbances and executive dysfunction. These problems can hinder the person’s ability to process information, make decisions and carry out everyday tasks effectively. We will look in more detail later at what these symptoms consist of.
Social functioning is also affected in schizophrenia. Difficulties in maintaining interpersonal relationships, participating in social activities and meeting work or academic responsibilities are common among those who suffer from this disorder (Belloch et al., 2020). This can lead to social isolation and a decline in quality of life.
Although the exact cause of schizophrenia is not yet fully known, it is estimated that it results from a combination of genetic, biological and environmental factors (Gejman and Sanders, 2012). Imbalances in neurotransmitters such as dopamine and serotonin in the brain have also been linked to schizophrenia, as well as certain structural neurological alterations (Ramírez-Jirano et al., 2019).
With regard to its treatment, it generally involves several professionals in a multidisciplinary setting. On the one hand, there is pharmacological treatment, which usually consists of antipsychotics, together with psychological therapy, social support and neuropsychological intervention. Medications can help control psychotic symptoms, while therapy can help the person learn to manage symptoms, improve social skills and regain a certain degree of functionality.
However, it is important to emphasize that schizophrenia is a complex disorder and that treatment may vary according to the individual needs of each person. The support of family, friends and mental health professionals also plays a crucial role in the recovery and management process of the illness.

Subscribe
to our
Newsletter
Types of schizophrenia
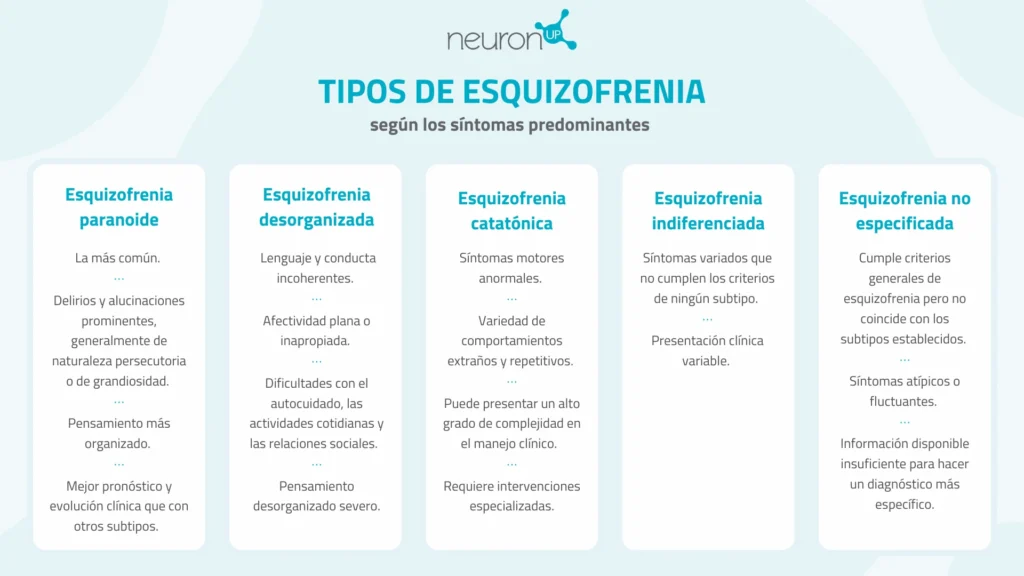
Traditionally, schizophrenia has been classified into several subtypes according to the predominant symptoms presented by the affected person. One of the most common subtypes is paranoid schizophrenia, where delusions and hallucinations are prominent, generally of a persecutory or grandiose nature. People with this subtype tend to have a better prognosis and clinical course compared to other subtypes.
Another important subtype is disorganized schizophrenia, characterized by incoherent speech and behavior, as well as flattened or inappropriate affect. People with this subtype may have difficulty performing everyday activities and maintaining meaningful social relationships due to the lack of organization in their thinking and behavior.
There is also catatonic schizophrenia, which is characterized by the presence of abnormal motor symptoms, such as muscle rigidity, immobility or excessive agitation. People with this subtype may display a variety of strange and repetitive behaviors, such as unusual postures or repetitive movements without apparent purpose. Although less common today due to advances in treatment, catatonic schizophrenia can present a high degree of complexity in clinical management and requires specialized interventions.
On the other hand is undifferentiated schizophrenia, a term used to describe cases in which the symptoms do not meet clear criteria for any specific subtype of schizophrenia. In these cases, the clinical presentation may be variable and does not fit a distinctive profile.
Finally, unspecified schizophrenia is used when the clinical presentation does not clearly match any of the established subtypes of schizophrenia, but still meets the general diagnostic criteria for the disorder. This category is used when the available information is insufficient to make a more specific diagnosis or when the symptoms are atypical or fluctuating.
However, it should also be noted that current nosological systems (DSM-5-TR and ICD-11) advocate not differentiating between these types, and point to a single typology where there may be a predominance of one characteristic or another (Valle, 2020).
Neuropsychological symptoms of schizophrenia
As we have seen, schizophrenia not only manifests through psychotic symptoms such as hallucinations and delusions, but also presents a variety of cognitive dysfunctions that affect the thinking, attention and memory abilities of those who suffer from it. These neuropsychological symptoms are fundamental to understanding the complexity of the illness and its impact on the daily lives of affected individuals.
One of the most prominent neuropsychological symptoms in schizophrenia is memory impairment. Patients may experience difficulties remembering recent information or retrieving long-term memories (Henry et al., 2019). This deficit can manifest in everyday situations, such as forgetting important tasks or having difficulty following conversations
Attention is another cognitive function affected in schizophrenia. Patients may have difficulty staying focused on a task or filtering out irrelevant stimuli from the environment (Hare, 2021). This can lead to reduced academic or work performance, as well as problems in social interactions due to lack of attention toward others.
Executive dysfunction is a common neuropsychological symptom in schizophrenia. This refers to difficulties in planning, organizing, decision-making and problem-solving (Sheffield et al., 2018). Patients may have difficulty setting realistic goals or carrying out complex tasks efficiently, which affects their ability to function independently in daily life.
Thought disorders, such as disorganized thought or lack of verbal fluency, are distinctive characteristics of schizophrenia. These neuropsychological symptoms manifest in the way patients process and express information, which can hinder effective communication and the understanding of abstract ideas (Ojeda, 2018).
In addition to affecting cognitive functions, the neuropsychological symptoms of schizophrenia also have a significant impact on individuals’ social functioning. Difficulties remembering past conversations, maintaining attention during social interactions and processing social information can make it difficult to establish and maintain meaningful relationships.
How clinical neuropsychology intervenes in schizophrenia
In the field of clinical neuropsychology various strategies are used to address the symptoms of schizophrenia. These can include cognitive-behavioral therapies, social skills training and cognitive rehabilitation programs.
It should be noted that neuropsychological intervention in schizophrenia is an integral part of treatment. This therapeutic modality, let us remember, focuses on understanding and addressing the cognitive deficits associated with schizophrenia as seen in the previous section.
Neuropsychological intervention is adapted to the individual needs of each patient, using techniques and strategies designed to improve cognitive function and, ultimately, the quality of life of the patient and their relatives.
An important approach in neuropsychological intervention is cognitive rehabilitation, which seeks to improve compromised cognitive skills through the repeated and structured practice of specific tasks (Skokou et al, 2023). These tasks can include exercises for memory, attention and problem solving, adapted to the abilities and goals of each individual.
Such cognitive rehabilitation helps people with schizophrenia recover or improve their cognitive functioning, which in turn can have a positive impact on their ability to carry out daily activities and participate in society.
In addition to traditional cognitive rehabilitation, the use of digital tools and programs can be beneficial in neuropsychological intervention for schizophrenia. In this way, NeuronUP constitutes a platform that offers a wide range of activities specifically designed for cognitive rehabilitation, including exercises to improve memory, attention, concentration and other cognitive functions. These digital tools can be especially useful for providing a personalized and scalable intervention, allowing neuropsychologists to tailor treatment to the specific needs of each patient and adequately monitor their progress over time.
Finally, throughout the intervention process it is highly advisable to involve the patient’s family, both in early stages to carry out proper psychoeducation about the disorder and associated deficits, and to achieve good treatment adherence by the patient throughout the intervention.
Future perspectives
The future perspectives in the neuropsychological treatment of schizophrenia are marked by an increasingly personalized and neuroscience-based approach. Advances in understanding the neurobiological mechanisms underlying the disease are expected to lead to more specific and effective therapies aimed at the characteristic cognitive deficits of schizophrenia.
One promising area is the development of pharmacological and non-pharmacological interventions intended to modulate brain function in individuals with schizophrenia. New classes of drugs that act on neurotransmitter systems involved in the cognitive symptoms of the disease, such as dopamine, glutamate and acetylcholine, are being investigated. In addition, emerging neuromodulation therapies, such as deep brain stimulation and transcranial magnetic stimulation (Mehta et al., 2019), are being explored as ways to modulate brain activity and improve cognitive function in schizophrenia.
Another important approach is the integration of digital technology into cognitive rehabilitation of patients with schizophrenia. The development of more sophisticated applications and software programs, specifically tailored to the individual needs of patients, is expected to improve the accessibility and effectiveness of neuropsychological intervention. These tools can provide a scalable and cost-effective way to offer personalized therapies, allowing patients to participate in cognitive rehabilitation from the comfort of their homes and facilitating remote monitoring by health professionals.
Furthermore, ongoing research into cognitive and neurobiological biomarkers in schizophrenia may facilitate the development of more precise and earlier treatment approaches (Perkovic et al., 2017). The identification of specific biological markers that predict the progression of cognitive symptoms could allow targeted preventive interventions aimed at preserving brain function and preventing long-term cognitive decline in people at risk of developing schizophrenia or in the early stages of the disease.
Together, these future perspectives in the neuropsychological treatment of schizophrenia offer a very broad scenario, filled with significant advances in the understanding and management of the cognitive deficits associated with this disease. With a multidisciplinary approach that integrates the latest advances in neuroscience, pharmacology and digital technology, it is possible that in the future there will be more effective and personalized therapeutic options to improve the quality of life of people affected by schizophrenia.
In conclusion, neuropsychology offers a very enriching — and in many cases necessary — perspective for understanding and treating schizophrenia. By addressing the cognitive and emotional problems associated with this disease, neuropsychologists can improve the quality of life of affected individuals and advance the field of mental health.
Bibliography
- American Psychiatric Association (APA) (2022). Diagnostic and Statistical Manual of Mental Disorders (5th Edition, Text Revision) (DSM-5-TR). Médica Panamericana Publishing.
- Belloch, A., Sandín, B., and Ramos, F. (2020). Manual of Psychopathology. Volume II (3rd ed.). McGrawHill Publishing.
- Gejman, P. V., and Sanders, A. R. (2012). The etiology of schizophrenia. Medicina, 72(3), 227–234.
- Hare S. M. (2021). Hallucinations: A Functional Network Model of How Sensory Representations Become Selected for Conscious Awareness in Schizophrenia. Frontiers in neuroscience, 15, 733038. https://doi.org/10.3389/fnins.2021.733038
- Ojeda, N. (2018). Neuropsychology of schizophrenia. Síntesis Publishing.
- Henry, J. D., Moore, P., Terrett, G., Rendell, P. G., & Scott, J. G. (2019). A comparison of different types of prospective memory reminders in schizophrenia. Schizophrenia research, 210, 89–93. https://doi.org/10.1016/j.schres.2019.06.002
- Mehta, U. M., Naik, S. S., Thanki, M. V., & Thirthalli, J. (2019). Investigational and Therapeutic Applications of Transcranial Magnetic Stimulation in Schizophrenia. Current psychiatry reports, 21(9), 89. https://doi.org/10.1007/s11920-019-1076-2
- Perkovic, M. N., Erjavec, G. N., Strac, D. S., Uzun, S., Kozumplik, O., & Pivac, N. (2017). Theranostic Biomarkers for Schizophrenia. International journal of molecular sciences, 18(4), 733. https://doi.org/10.3390/ijms18040733
- Ramírez-Jirano, L. J., Velasco-Ramírez, S. F., Pérez-Carranza, G. A., Domínguez-Díaz, C., & Bitzer-Quintero, O. K. (2019). Cytokines and the nervous system: relationship with schizophrenia. Revista médica del Instituto Mexicano del Seguro Social, 57(2), 107–112.
- Sheffield, J. M., Karcher, N. R., & Barch, D. M. (2018). Cognitive Deficits in Psychotic Disorders: A Lifespan Perspective. Neuropsychology review, 28(4), 509–533. https://doi.org/10.1007/s11065-018-9388-2
- Skokou, M., Messinis, L., Nasios, G., Gourzis, P., & Dardiotis, E. (2023). Cognitive Rehabilitation for Patients with Schizophrenia: A Narrative Review of Moderating Factors, Strategies, and Outcomes. Advances in experimental medicine and biology, 1423, 193–199. https://doi.org/10.1007/978-3-031-31978-5_17
- Valle R. (2020). Schizophrenia in ICD-11: Comparison of ICD-10 and DSM-5. La esquizofrenia en la CIE-11: comparación con la CIE-10 y el DSM-5. Revista de psiquiatría y salud mental, 13(2), 95–104. https://doi.org/10.1016/j.rpsm.2020.01.001
If you enjoyed this article about the neuropsychology of schizophrenia, you will surely be interested in these NeuronUP articles:
“This article has been translated. Link to the original article in Spanish:”
Neuropsicología de la esquizofrenia






 Understanding Dysgraphia
Understanding Dysgraphia
Leave a Reply