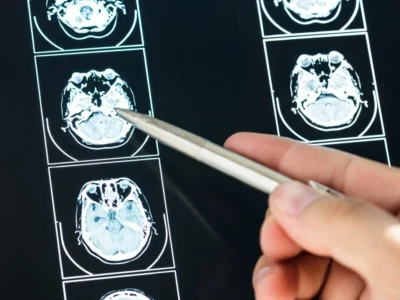
Neuropsychologist Estefanía Lesser explains the impact of depression on cognition and why cognitive stimulation is crucial for older adults with depression.
Introduction
“Aging” is a natural process that involves biological, psychological and social transformations, many of which directly affect the mental health of older adults. In this context, depression in old age has become a growing and often underestimated problem. Its manifestations often differ from those observed in other stages of life, and its effects are not limited to the emotional realm but also significantly impact cognitive functions, such as memory, attention and executive functions.
Despite its high prevalence, depression in older adults continues to be underdiagnosed, especially when it presents with atypical symptoms or is confused with cognitive impairment. This overlap can lead to conditions such as depressive pseudodementia, where the cognitive impairment is secondary to depression and potentially reversible. Given this panorama, it becomes urgent to implement therapeutic strategies that integrate emotional treatment with the preservation of cognitive functions.
Among these strategies, cognitive stimulation has become established as an effective intervention, with scientific evidence supporting its ability to improve cognitive performance, strengthen self-esteem, reduce isolation and prevent neurocognitive decline. Its positive impact is further enhanced when it is part of a multidisciplinary approach involving neuropsychologists, clinical psychologists, occupational therapists, speech therapists, physiotherapists, psychiatrists and caregivers.
Depression in older adults and its impact on cognition
What depression is
Depression is a mood disorder that involves a combination of emotional, physical and cognitive symptoms, including persistent sadness, loss of interest, sleep disturbances, fatigue, difficulty concentrating and recurrent negative thoughts (American Psychiatric Association, 2013). In older adults, this condition often goes unnoticed due to atypical manifestations such as apathy, slowness or somatic complaints (González-Fernández et al., 2020).
Prevalence of depression in older adults
The prevalence of depression in older adults is estimated to range between 10% and 15% in the general population, but it can reach between 20% and 25% in institutionalized people or those with chronic illnesses (Pérez-Arechaederra et al., 2018; World Health Organization [WHO], 2017).
In the Latin American context, studies such as the SABE Survey in Colombia have reported prevalences even higher than 30% in people over 60 years old (Albala et al., 2005).
Clinical identification of depression in older adults
For clinical identification, instruments such as the Geriatric Depression Scale (GDS), the Beck Depression Inventory-II adapted for older adults and structured interviews such as the Mini International Neuropsychiatric Interview (MINI) are used. These tests allow effective screening adjusted to the cognitive and emotional profile of this population (Yesavage et al., 1982; González et al., 2013).
Symptoms of depression in young and older adults
In older adults, depressive symptoms can differ from those observed in younger adults. They may present apathy, irritability, loss of energy, functional difficulties, social withdrawal and persistent somatic complaints (Blazer, 2003; Jeste et al., 1999). These symptoms not only affect emotional state but also performance on cognitive tasks, particularly in executive functions such as planning, working memory, sustained attention and inhibitory control (Butters et al., 2004; Sachs-Ericsson et al., 2011).
What depressive pseudodementia is
A relevant condition in this context is depressive pseudodementia, a clinical syndrome in which depressive symptoms mimic severe cognitive impairment. Unlike neurodegenerative dementias such as Alzheimer’s, in pseudodementia the cognitive deficits do not progress and can be reversible with appropriate treatment (Ritchie et al., 1994; Looi & Macfarlane, 2009). Patients are often aware of their difficulties and tend to dramatize them, which contrasts with the typical anosognosia of dementia. However, it is important to note that some patients with pseudodementia may progress to irreversible dementia if not intervened in time (Barnes et al., 2006).

Subscribe
to our
Newsletter
Why cognitive stimulation is crucial for older adults with depression
Cognitive stimulation comprises a set of therapeutic techniques that seek to maintain or improve the functioning of cognitive functions. In older adults with depression, these interventions are not only recommended but necessary, due to their effect on multiple dimensions of well-being.
1. Neuroplasticity in old age
Although brain plasticity decreases with age, the brain remains capable of adapting, generating new synaptic connections and reorganizing neural networks in response to environmental stimuli and cognitive training (Park & Bischof, 2013; Draganski & May, 2008). This principle underlies the effectiveness of cognitive stimulation by promoting the activation of areas compromised by depression and compensating for impaired functions. Additionally, it has been shown that even in aged brains, learning new skills can induce lasting functional and structural changes (Valenzuela & Sachdev, 2009).
2. Reducing the impact of depression on cognitive functioning
Active participation in cognitive exercises helps to counteract the mental slowing and loss of initiative typical of depressive episodes, favoring motivation and concentration (Bennett & Thomas, 2014). This type of intervention can relieve cognitive symptoms secondary to depression and improve daily functional performance.
3. Improvement of emotional well-being
Regular practice of cognitive stimulation gives the older adult an opportunity to experience personal achievements, overcome challenges and regain a sense of competence. These factors raise self-esteem and reduce feelings of worthlessness or hopelessness, common in geriatric depression (Cummings et al., 2019).
4. Prevention of greater cognitive decline
Depression in old age is associated with an increased risk of mild cognitive impairment and dementia (Ownby et al., 2006). Therefore, early interventions such as cognitive stimulation not only treat current symptoms but can help slow future cognitive decline.
Conclusion
In view of these findings, in the second part of this article we will delve into the specific benefits of cognitive stimulation, concrete strategies for clinical application and the role of the interdisciplinary team and caregivers in this therapeutic process.
If you are interested in learning more about cognitive stimulation in older adults with depression, you can continue reading the second part of this article here.
Bibliography
- Albala, C., et al. (2005). Aging and health conditions in Latin America: results of the SABE study. Pan American Health Organization.
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing.
- Barnes, D. E., Alexopoulos, G. S., Lopez, O. L., Williamson, J. D., & Yaffe, K. (2006). Depressive symptoms, vascular disease, and mild cognitive impairment: findings from the Cardiovascular Health Study. Archives of General Psychiatry, 63(3), 273–279. https://doi.org/10.1001/archpsyc.63.3.273
- Blazer, D. G. (2003). Depression in late life: Review and commentary. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 58(3), 249–265. https://doi.org/10.1093/gerona/58.3.m249
- Cummings, J. L., Lyketsos, C. G., & Sweet, R. A. (2019). Cognitive and behavioral aspects of aging: A clinical guide. Oxford University Press.
- Draganski, B., & May, A. (2008). Training-induced structural changes in the adult human brain. Behavioural Brain Research, 192(1), 137–142. https://doi.org/10.1016/j.bbr.2008.02.015
- González-Fernández, M., Moreno-Peral, P., Conejo-Cerón, S., Motrico, E., & Bellón, J. Á. (2020). Clinical characteristics and prognosis of depression in the older adult. Atención Primaria, 52(9), 598–607. https://doi.org/10.1016/j.aprim.2019.09.008
- Looi, J. C. L., & Macfarlane, M. D. (2009). Pseudodementia: Can depressive pseudodementia be distinguished from Alzheimer’s disease using specific clinical features? International Journal of Geriatric Psychiatry, 24(5), 469–475. https://doi.org/10.1002/gps.2142
- Park, D. C., & Bischof, G. N. (2013). The aging mind: Neuroplasticity in response to cognitive training. Dialogues in Clinical Neuroscience, 15(1), 109–119. https://doi.org/10.31887/DCNS.2013.15.1/dpark
- Pérez-Arechaederra, D., et al. (2018). Depression in older people. Revista Española de Geriatría y Gerontología, 53(2), 91–98. https://doi.org/10.1016/j.regg.2017.06.002
- Ritchie, K., Artero, S., & Touchon, J. (1994). Classification criteria for mild cognitive impairment: A population-based validation study. Neurology, 56(1), 37–42. https://doi.org/10.1212/WNL.56.1.37
- Valenzuela, M. J., & Sachdev, P. (2009). Can cognitive exercise prevent the onset of dementia? Systematic review of randomized clinical trials with longitudinal follow-up. The American Journal of Geriatric Psychiatry, 17(3), 179–187. https://doi.org/10.1097/JGP.0b013e3181953b57
- Yesavage, J. A., et al. (1982). Development and validation of a geriatric depression screening scale: A preliminary report. Journal of Psychiatric Research, 17(1), 37–49. https://doi.org/10.1016/0022-3956(82)90033-4
Frequently asked questions about the placebo effect
1. What is the relationship between depression and cognitive impairment in older adults?
Depression can cause impairment in cognitive functions such as memory, attention and executive functions. In some cases, these symptoms are confused with dementia, as happens in depressive pseudodementia.
2. What is depressive pseudodementia?
It is a syndrome in which depressive symptoms mimic severe cognitive impairment, but are reversible with appropriate treatment. Unlike dementia, there is no neurodegenerative progression.
3. Why is it difficult to diagnose depression in older adults?
Symptoms can be atypical: somatic complaints, apathy or slowness. In addition, it tends to be confused with normal aging or mild cognitive impairment.
4. How is depression diagnosed in older people?
With tools such as the Geriatric Depression Scale (GDS), the adapted Beck Inventory and structured interviews such as the MINI.
5. Which professionals should intervene in a case of depression with cognitive impairment?
The approach should be multidisciplinary and include neuropsychologists, clinical psychologists, psychiatrists, occupational therapists and primary care physicians.
If you enjoyed this article about depression in older adults, you may also be interested in these NeuronUP articles:
“This article has been translated. Link to the original article in Spanish:”
La depresión en adultos mayores: impacto cognitivo y abordaje desde la estimulación




 Placebo Effect in Cognitive Stimulation: What It Is, Scientific Evidence, and Clinical Keys for Applying It in Neurorehabilitation
Placebo Effect in Cognitive Stimulation: What It Is, Scientific Evidence, and Clinical Keys for Applying It in Neurorehabilitation
Leave a Reply