José López Sánchez, coordinator of therapies at CEN, presents in this article cognitive-motor training based on dual tasks, virtual reality and augmented reality.
(This document “Cognitive-motor training: use of dual tasks, virtual reality and augmented reality” is based on a free translation of the document entitled “Gait and balance training based on virtual and augmented reality” (1) with contributions from the author José López Sánchez, based on his clinical experience and other scientific studies published on the subject.)
Introduction
- The use of virtual reality and augmented reality in neurorehabilitation has become popular in recent years and has received great attention in the scientific literature (around 1,000 articles) (1).

- Deficits in cognitive-motor dual tasks (for example, walking while talking) are common in people with neurological sequelae. Cognitive-motor dual-task training has been proposed as an alternative to conventional rehabilitation methods when addressing these problems (2).
- The results of studies on dual-task training show improvements in:
- Gait speed in a single task, and step length in people with Parkinson’s disease and Alzheimer’s disease.
- Gait speed in dual tasks in people with Parkinson’s disease, Alzheimer’s disease and brain injury.
- It could improve balance and cognition of people with Parkinson’s disease and Alzheimer’s disease.
Principles of treatment
The protocols used in the different studies and the outcome measures employed are still very heterogeneous and do not allow comparison between groups. Nevertheless, training should follow a set of principles that, following motor learning theories, allow interventions to be optimized and results to be improved.
These principles that we should apply in training would be:
- Attentional focus,
- implicit learning,
- variation,
- training intensity,
- task specificity,
- feedback.
We will explain the treatment principles one by one:
1. Attentional focus
During rehabilitation, therapists need to explain exercises to patients, and the instructions they provide will influence the patient’s attentional focus, the execution of the movement and its outcome.
Often therapists use instructions referring to body parts or movements (for example, keep your knees behind your toes, to promote greater knee extension). In motor learning this is known as “instructions that promote an internal focus of attention”. This causes more conscious movements that interfere with automatic motor control (3).
Furthermore, in people with attentional problems, it consumes a large part or all of the person’s attentional capacity, leaving no resources to cope with other tasks at the same time (dual tasks).
Recent studies indicate that instructions that promote an external focus, for example directing attention to the effect of the movement on the environment (for example “touch the mark on the floor with your foot”), achieve an improvement in motor learning.
Studies carried out in sport (4-6) and balance training (7) consistently show better motor performance after a period of learning focused on an external focus, versus instructions centered on an internal focus. However, in daily practice it is sometimes difficult to find the right instructions that induce an external attentional focus.

One of the advantages of augmented reality is that it can facilitate gait adjustments, for example, through the external cues it provides, such as targets that the patient must step on, projected onto the surface they walk on, or auditory cues.
In this case, augmented reality using external cues directs the patient’s attentional focus to the virtual world, instead of to the patient’s body, which promotes an external attentional focus and will likely improve the therapy outcome, according to motor learning principles.
2. Implicit learning
Traditionally, new motor skills are taught through explicit instructions, resulting in conscious control of the movement. However, movement control is usually based on implicit knowledge. We know how to perform the movement, but we are usually not aware of how we control our muscles and cannot explain it in words.
Recent studies suggest that explicit learning can limit or interfere with these automatic processes, leading to poorer performance, especially when people have to perform a task under pressure (8-12). Rehabilitation could therefore benefit from the use of implicit learning, for example, learning without awareness of what is being learned.
For example, in patients after suffering a stroke, performance of a dynamic balance task was worse after a period of explicit learning versus implicit learning (13). Previously, a way to promote implicit learning has been described through instructions or tasks that require an external focus of attention.
Another alternative is through the use of a concurrent cognitive task (dual task) (9) or through variation in tasks, in such a way that learning through explicit rules is impossible. Virtual and augmented reality games often promote this implicit learning through one or more of these principles.
Definitely, it is time to change old paradigms in neurorehabilitation where the patient goes to physiotherapy or occupational therapy when they want to work on motor aspects of the leg or arm and to the neuropsychologist when they want to work on cognitive aspects. The scientific evidence shows us the constant interaction of cognitive and motor aspects and the interaction between the patient’s abilities, the task and the environment are key for relearning.
That is why we must think about what type of learning the task we present to the patient is promoting and the environment in which they will perform it, adjusting it to their abilities so they can progress as the patient practices and improves.
3. Variation
The importance of variation in exercises is another lesson we have learned from research in the field of motor learning.
Instead of training the exact same movement over and over, small variations in the movement will result in more robust motor learning (14). In addition, variations in the sequence of exercises (random versus blocked) will improve motor learning, especially retention and transfer (15).
Although studies consistently favor variable practice, most have focused on laboratory tasks (15,16) or sports applications (14, 17-19).
When these principles are applied, for example, to balance training, postural sway in standing is reduced after 15 minutes of varied balance exercises (weight transfer exercises and reduced bases of support) whereas no difference is found after repetitive training or simply standing still (20).
Therefore, it seems that variable practice of tasks can also improve outcomes in rehabilitation. Through the use of virtual or augmented reality, variations can be easily created by modifying the numerous parameters of the exercises, such as target placement, speed requirements, environmental elements, etc.
4. Training intensity
Training intensity (number of repetitions, training frequency, task difficulty, etc.) is a determining factor of the therapy outcome (21-23). High-intensity training is recommended to maximize the effect of treatment.
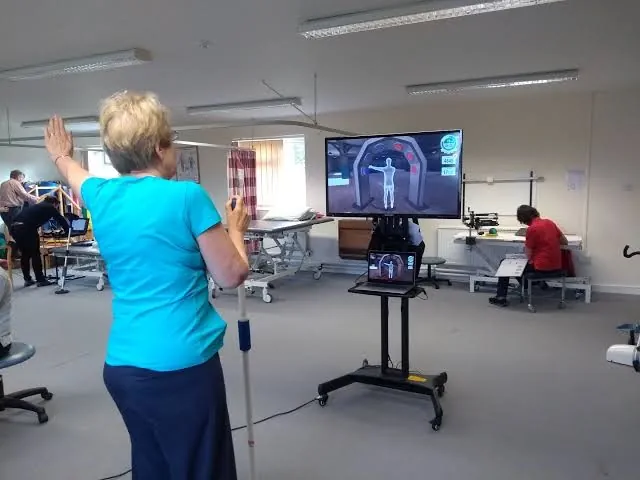
Virtual and augmented reality could help achieve high practice intensities by increasing some patients’ motivation and their adherence to treatment, improving training efficiency and providing an appropriate challenge.
In addition, virtual and augmented reality (VR and AR) enable two types of training: independent training by the patient, in the clinic and at home.
In many rehabilitation centers the patient/therapist ratio is low and that poses a challenge when increasing training intensity. It also happens that many patients only practice when they are with the therapist, but when they return home they remain sedentary most of the time.
For these two situations VR and AR can be a solution for some patients, as they provide the feedback needed to carry out the exercises, these can be monitored remotely by a professional, adapted when necessary, and allow collection of information on how much activity the patient is doing and how they are performing it.
In neurorehabilitation repetitive training of relatively simple movement is often required. Certain exercises often become quickly boring, making it difficult for the patient to stay motivated and focused.
One of the benefits of virtual rehabilitation is the use of games, which for some patients can make therapy more fun and enjoyable (24-26). Some patients may engage more in the therapy session and increase treatment adherence (27-30).
Also, the number of repetitions that can be achieved and the active treatment time with virtual and augmented reality can be greater than with conventional therapy (31-33). For example, in one study twice as many steps were achieved during an AR and treadmill training task, compared with conventional gait training (31). Increased motivation is certainly one of the factors that explains this, but not the only one.
Other practical aspects, such as the lack of a physical need to assemble and modify different gait circuits, increase the time that, within a session, can be devoted to active training by the patient.
In addition, it is possible to control very precisely the level of challenge proposed to the patient based on their abilities. Game difficulty can be easily and gradually adapted, for example by changing speed requirements or distances of targets to be reached.
5. Task specificity
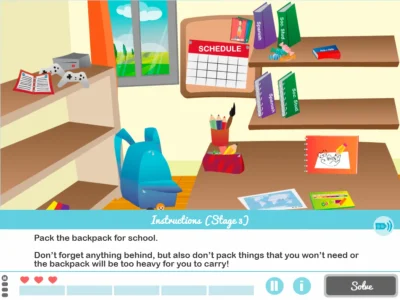
Another important recommendation for rehabilitation is to include task-specific training (22, 34). To improve transfer of motor function gains to activities outside therapy, therapy should include practice of everyday life challenges. VR and AR can be used to simulate such challenges in a safe environment.
For example, virtual and augmented reality could help train walking in difficult situations. This is essential, because walking in daily life is much more than putting one foot in front of the other; it also requires the ability to adjust gait patterns to different situations.
You may need to lift your leg higher to avoid tripping on a loose paving stone, or slow down to avoid bumping into someone, or speed up to catch a traffic light that is turning amber, or weave around people in a crowded shopping mall.
Gait adaptability is defined as the agility to adjust gait according to environmental circumstances, and is therefore a crucial element when walking at home and especially in the community.
AR can be a useful tool to train gait adaptability, projecting foot targets or obstacles onto the surface being walked on (35,36). In addition, virtual reality can be used to create an optic flow when walking on a treadmill, to improve the natural sensation of walking (37,38).
Other examples of everyday challenges are activities that comprise cognitive and motor tasks at the same time, such as crossing a street paying attention to traffic, or walking while remembering what you needed to buy at the supermarket, or while conversing with a friend.
When two tasks are performed simultaneously, the quality and execution of one or both tasks may be reduced. This is known as “dual-task interference”, which occurs more often with age (39), and with some neurological conditions such as stroke (40) or Parkinson’s disease (41).
Dual-task interference has been shown to be a predictor of falls (42). Training in dual tasks is more effective at reducing “dual-task interference” than single-task training (43-46) and therefore fall prevention programs should always include dual tasks (47).
Through virtual reality it is relatively easy to add cognitive elements to training, and thus dual-task training. One way to do this is to include a cognitive task that is not related to the motor task, for example counting backwards or a memory task.
In the vast majority of cases, cognitive training is done seated at a table, rarely in motion. It would be very interesting to include the use of stimulation systems and cognitive rehabilitation at the same time as walking, practicing balance exercises, or simply standing.
Another way to incorporate the cognitive task within the virtual reality game, for example, is through games that require planning or development of a strategy.
Finally, cognitive elements can be added by simulating dual-task challenges that occur in everyday life, such as walking in a virtual supermarket while placing a series of items in the shopping cart (48) or crossing the street while avoiding obstacles (49).
6. Feedback
To improve our motor performance we need at least some kind of information about how we are performing a task. This feedback or reNutrition often comes from intrinsic sources, such as vision or proprioception.
Intrinsic feedback can be increased by providing information that would normally be inaccessible to the patient, such as the exact angles of joints or movements (biofeedback).
Through virtual reality, biofeedback can be shown to the patient or even incorporated into the exercise. Providing biofeedback can be very useful for gait or balance training.
Balance training with feedback normally consists of weight transfer exercises in which the patient receives information about the position of their center of pressure.
In a systematic review, the effectiveness of feedback-based balance training in older adults was evaluated and it was concluded that such training results in reduced postural sway, improved weight transfer ability, reduced attentional demands while standing still and improved scores on the Berg scale (50).
There is also some evidence suggesting that adding biofeedback to balance training in people with sequelae after stroke can be beneficial (51,52).
There is a large literature showing the effectiveness of biofeedback for gait retraining in different patient populations. For example, feedback training can reduce knee adduction movement or increase toe angle for knee osteoarthritis prevention (53-55).
It can also improve propulsion during push-off in healthy older adults, making their gait pattern more similar to that of young adults (56).
Feedback can help people with Parkinson’s disease, or incomplete spinal cord injury to take longer steps (57,58) and improve gait in people after a transfemoral amputation (59). It has been seen that it can help modulate gait parameters in children with cerebral palsy (60). There are other applications to prevent running injuries, knee hyperextension patterns (61,62), etc.

All these examples show how biofeedback is an effective and versatile tool that allows patients to adapt specific aspects of their gait. In conclusion, the ability to provide biofeedback is one of the great advantages of VR training. By incorporating augmented feedback into a game you can increase patient motivation and engagement.
Conclusions
- Virtual reality and augmented reality are tools that can help make our training more specific, effective and motivating for the patient.
- We must know why, for what and how we use VR and AR. The use of these technologies does not simply mean putting VR goggles on a person and having them perform tasks, or putting them in front of a screen to play. We must think about why we use these tools, that is, what they provide us that is special and distinctive compared to not using them or compared to other forms of treatment. Then we must think about which specific aspect of the treatment we are going to use them for: improving movement information through biofeedback, cognitive training in dual tasks, training daily life situations, etc. And finally, we must think about how we are going to use them: following the six treatment principles explained in this text.
- It is advisable to design treatments that combine motor and cognitive aspects. As discussed throughout the text, VR and AR, together with other systems and platforms of cognitive rehabilitation, can be used jointly with gait training, balance training, or upper limb training, to name just a few.
Bibliography
- Virtual and Augmented reality based balance and gait training. Selma Papegaaij, Floris Morang, Frans Steenbrink. https://www.hocoma.com/news/virtual-augmented-reality-based-balance-gait-training/
- Motor-Cognitive Dual-Task Training in Persons With Neurologic Disorders: A Systematic Review. Fritz NE, Cheek FM, Nichols-Larsen DS. https://www.ncbi.nlm.nih.gov/pubmed/26079569
- The automaticity of complex motor skill learning as a function of attentional focus. Wulf G, McNevin N, Shea CH. https://www.ncbi.nlm.nih.gov/pubmed/11765737
- Increased movement accuracy and reduced EMG activity as the result of adopting an external focus of attention. Zachry T, Wulf G, Mercer J, Bezodis N. https://www.ncbi.nlm.nih.gov/pubmed/16182938
- Enhancing the Learning of Sport Skills Through External-Focus Feedback. Wulf G, Mcconnel N, Gärtner M, Schwarz A. https://www.ncbi.nlm.nih.gov/pubmed/12057890
- The effects of attentional focusing strategies on novice dart throwing performance and Their task experiences. Marchant DC, Clough PJ, Crawshaw M. https://www.tandfonline.com/doi/abs/10.1080/1612197X.2007.9671837
- Effects of external focus of attention on balance: a short review. Park SH, Yi CW, Shin JY, Ryu YU. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4713821/
- Reinvestment and movement disruption following stroke. Orrell AJ, Masters RSW, Eves FF. https://www.ncbi.nlm.nih.gov/pubmed/18987385
- Knowledge, knerves and know-how: The role of explicit versus implicit knowledge in the breakdown of a complex motor skill under pressure. Masters R. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.2044-8295.1992.tb02446.x
- The role of reinvestment in walking and falling in community- dwelling older adults. Wong W-L, Masters RSW, Maxwell JP, Abernethy B. https://onlinelibrary.wiley.com/doi/full/10.1111/j.1532-5415.2009.02228.x
- Duration of Parkinson disease is associated with an increased propensity for “reinvestment”. Masters RSW, Pall HS, MacMahon KMA, Eves FF. https://www.ncbi.nlm.nih.gov/pubmed/17312087
- Analogy learning: A means to implicit motor learning. Liao C-M, Masters RSW. https://www.ncbi.nlm.nih.gov/pubmed/11354610
- Motor learning of a dynamic balancing task after stroke: implicit implications for stroke rehabilitation. Orrell AJ, Eves FF, Masters RSW. https://academic.oup.com/ptj/article/86/3/369/2805183
- A quantitative dynamical systems approach to differential learning: self-organization principle and order parameter equations. Frank TD, Michelbrink M, Beckmann H, Schöllhorn WI. https://www.ncbi.nlm.nih.gov/pubmed/18026746
- Contextual interference effects on the acquisition, retention, and transfer of a motor skill. Shea J, Morgan R. https://psycnet.apa.org/record/1980-24610-001
- Programming and reprogramming sequence timing following high and low contextual interference practice. Wright DL, Magnuson CE, Black CB. https://www.ncbi.nlm.nih.gov/pubmed/16270703
- Does noise provide a basis for the unification of motor learning theories?. Schollhorn W, Beckmann H. https://psycnet.apa.org/record/2006-22320-007
- Differencial learning in shot put. Beckmann H, Schöllhorn WI. https://www.researchgate.net/publication/291047775_Differential_learning_in_shot_put_Differential_learning_in_shot_put
- Contextual interference effects with skilled baseball players. Hall KG, Domingues DA, Cavazos R. https://www.ncbi.nlm.nih.gov/pubmed/8084699
- Short-term differential training decreases postural sway. James EG. https://www.ncbi.nlm.nih.gov/pubmed/23877033
- Potential Contributions of Training Intensity on Locomotor Performance in Individuals With Chronic Stroke. Holleran CL, Rodriguez KS, Echauz A, Leech KA, Hornby TG. https://www.ncbi.nlm.nih.gov/pubmed/25784587
- Stroke rehabilitation. Langhorne P, Bernhardt J, Kwakkel G. https://www.ncbi.nlm.nih.gov/pubmed/21571152
- Effects of Balance Training on Balance Performance in Healthy Older Adults: A Systematic Review and Meta-analysis. Lesinski M, Hortobagyi T, Muehlbauer T, Gollhofer A, Granacher U. https://www.ncbi.nlm.nih.gov/pubmed/26325622
- A controlled pilot trial of two commercial video games for rehabilitation of arm function after stroke. Chen M-H, Huang L-L, Lee C-F, et al. https://www.ncbi.nlm.nih.gov/pubmed/25322868
- Effectiveness of conventional versus virtual reality-based balance exercises in vestibular rehabilitation for unilateral peripheral vestibular loss: results of a randomized controlled trial. Meldrum D, Herdman S, Vance R, et al. https://www.ncbi.nlm.nih.gov/pubmed/25842051
- Efficacy of virtual reality-based balance training versus the Biodex balance system training on the body balance of adults. Ibrahim MS, Mattar AG, Elhafez SM. https://www.ncbi.nlm.nih.gov/pubmed/26957722
- Exergaming With Additional Postural Demands Improves Balance and Gait in Patients With Multiple Sclerosis as Much as Conventional Balance Training and Leads to High Adherence to Home-Based Balance Training. Kramer A, Dettmers C, Gruber M. https://www.ncbi.nlm.nih.gov/pubmed/24823959
- Patient perspectives on virtual reality-based rehabilitation after knee surgery: Importance of level of difficulty. Lee M, Suh D, Son J, Kim J, Eun S-D, Yoon B. https://www.ncbi.nlm.nih.gov/pubmed/27149529
- Effects of virtual reality-enhanced exercise equipment on adherence and exercise-induced feeling states. Annesi JJ, Mazas J. https://www.ncbi.nlm.nih.gov/pubmed/9399288
- Usability and Effects of an Exergame-Based Balance Training Program. Wüest S, Borghese NA, Pirovano M, Mainetti R, van de Langenberg R, de Bruin ED. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3996993/
- Feasibility of C-mill gait-adaptability training in older adults after fall-related hip fracture: user’s perspective and training content. van Ooijen MW, Roerdink M, Timmermans C, et al. https://www.researchgate.net/publication/280269805_P268_Feasibility_of_C-mill_gait-adaptability_training_in_older_adults_after_fall-related_hip_fracture_user’s_perspective_and_training_content
- Eliciting Upper Extremity Purposeful Movements Using Video Games. Rand D, Givon N, Weingarden H, Nota A, Zeilig G. https://www.ncbi.nlm.nih.gov/pubmed/24515927
- Is upper limb virtual reality training more intensive than conventional training for patients in the subacute phase after stroke? An analysis of treatment intensity and content. Brunner I, Skouen JS, Hofstad H, et al. https://bmcneurol.biomedcentral.com/articles/10.1186/s12883-016-0740-y
- Understanding the pattern of functional recovery after stroke: facts and theories. Kwakkel G, Kollen B, Lindeman E. https://www.ncbi.nlm.nih.gov/pubmed/15502272
- Feasibility and Preliminary Efficacy of Visual Cue Training to Improve Adaptability of Walking after Stroke: Multi-Centre, Single- Blind Randomised Control Pilot Trial. Hollands KL, Pelton TA, Wimperis A, et al. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596478/
- Step by step: a proof of concept study of C-Mill gait adaptability training in the chronic phase after stroke. Heeren A, van Ooijen M, Geurts ACH, et al. https://www.ncbi.nlm.nih.gov/pubmed/23811818
- Effects of adding a virtual reality environment to different modes of treadmill walking. Sloot LH, van der Krogt MM, Harlaar J. https://www.ncbi.nlm.nih.gov/pubmed/24412269
- Self-paced versus fixed speed walking and the effect of virtual reality in children with cerebral palsy. Sloot LH, Harlaar J, van der Krogt MM. https://www.ncbi.nlm.nih.gov/pubmed/26338532
- Changes in Standing and Walking Performance Under Dual-Task Conditions Across the Lifespan. Ruffieux J, Keller M, Lauber B, Taube W. https://www.ncbi.nlm.nih.gov/pubmed/26253187
- Dual-task-related gait changes in individuals with stroke. Yang Y-R, Chen Y-C, Lee C-S, Cheng S-J, Wang R-Y. https://www.ncbi.nlm.nih.gov/pubmed/16650766
- Characterization of cognitive and motor performance during dual-tasking in healthy older adults and patients with Parkinson’s disease. Wild LB, de Lima DB, Balardin JB, et al. https://www.ncbi.nlm.nih.gov/pubmed/23052601
- Stops walking when talking: a predictor of falls in older adults?. Beauchet O, Annweiler C, Dubost V, et al. https://www.ncbi.nlm.nih.gov/pubmed/19473368
- Training effects on motor–cognitive dual-task performance in older adults. Wollesen B, Voelcker-Rehage C. https://link.springer.com/article/10.1007/s11556-013-0122-z
- The effect of single-task and dual-task balance exercise programs on balance performance in adults with osteoporosis: a randomized controlled preliminary trial. Konak HE, Kibar S, Ergin ES. https://www.ncbi.nlm.nih.gov/pubmed/27234670
- Virtual Reality Training with Cognitive Load Improves Walking Function in Chronic Stroke Patients. Cho KH, Kim MK, Lee H-J, Lee WH. https://www.ncbi.nlm.nih.gov/pubmed/26228205
- Multicomponent physical exercise with simultaneous cognitive training to enhance dual-task walking of older adults: A secondary analysis of a 6-month randomized controlled trial with I-year follow-up. Eggenberger P, Theill N, Holenstein S, Schumacher V, de Bruin ED. https://www.ncbi.nlm.nih.gov/pubmed/26604719
- Comparison of traditional and recent aproaches in the promotion of balance and strength in older adults. Granacher U, Muehlbauer T, Zahner L, Gollhofer A, Kressig RW. https://www.ncbi.nlm.nih.gov/pubmed/21510715
- Cognitive load and dual-task performance during locomotion poststroke: a feasibility study using a functional virtual environment. Kizony R, Levin MF, Hughey L, Perez C, Fung J. https://www.ncbi.nlm.nih.gov/pubmed/20023003
- A treadmill and motion coupled virtual reality system for gait training post-stroke. Fung J, Richards CL, Malouin F, McFadyen BJ, Lamontagne A. https://www.ncbi.nlm.nih.gov/pubmed/16640470
- Biofeedback for training balance and mobility tasks in older populations: a systematic review. Zijlstra A, Mancini M, Chiari L, Zijlstra W. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3019192/
- Influence of posturographic platform biofeedback training on the dynamic balance of adult stroke patients. Maciaszek J, Borawska S, Wojcikiewicz J. https://www.ncbi.nlm.nih.gov/pubmed/24774437
- Symmetrical body-weight distribution training in stroke patients and its effect on fall prevention. Cheng PT, Wu SH, Liaw MY, Wong AM, Tang FT. https://www.ncbi.nlm.nih.gov/pubmed/11733877
- Comparison of mirror, raw video, and real-time visual biofeedback for training toe-out gait in individuals with knee osteoarthritis. Hunt MA, Takacs J, Hart K, Massong E, Fuchko K, Biegler J. https://www.ncbi.nlm.nih.gov/pubmed/24910929
- Gait Retraining with real-time Biofeedback to reduce Knee adduction moment: systematic review of effects and methods used. Richards R, van den Noort JC, Dekker J, Harlaar J. https://www.ncbi.nlm.nih.gov/pubmed/27485366
- Real-time visual feedback for gait retraining: toward application in knee osteoarthritis. van den Noort JC, Steenbrink F, Roeles S, Harlaar J. https://www.ncbi.nlm.nih.gov/pubmed/25480419
- Real-time feedback enhances forward propulsion during walking in old adults. Franz JR, Maletis M, Kram R. https://www.ncbi.nlm.nih.gov/pubmed/24238977
- A System for Real-Time Feedback to Improve Gait and Posture in Parkinson’s Disease. Jellish J, Abbas JJ, Ingalls TM, et al. https://www.ncbi.nlm.nih.gov/pubmed/26316235
- Augmented multisensory feedback enhances locomotor adaptation in humans with incomplete spinal cord injury. Yen S-C, Landry JM, Wu M. https://www.ncbi.nlm.nih.gov/pubmed/24746604
- Gait training with virtual reality- based real-time feedback: improving gait performance following transfemoral amputation. Darter BJ, Wilken JM. https://www.ncbi.nlm.nih.gov/pubmed/21757579
- Real-time feedback to improve gait in children with cerebral palsy. van Gelder L, Booth ATC, van de Port I, Buizer AI, Harlaar J, van der Krogt MM. https://www.ncbi.nlm.nih.gov/pubmed/27883988
- Gait modifications to change lower extremity gait biomechanics in runners: a systematic review. Napier C, Cochrane CK, Taunton JE, Hunt MA. https://www.ncbi.nlm.nih.gov/pubmed/26105016
- Short and long-term effects of gait retraining using real-time biofeedback to reduce knee hyperextension pattern in young women. Teran-Yengle P, Cole KJ, Yack HJ. https://www.ncbi.nlm.nih.gov/pubmed/27637090
If you enjoyed this article about cognitive-motor training, you might also be interested in the following articles:
“This article has been translated. Link to the original article in Spanish:”
Entrenamiento cognitivo motor: uso de tareas duales, realidad virtual y aumentada






 The Confabulation Phenomenon (Vol. I): Classifications, Neuropathology, and Cognitive Mechanisms
The Confabulation Phenomenon (Vol. I): Classifications, Neuropathology, and Cognitive Mechanisms
Leave a Reply