María Alicia Lage, a psychologist licensed to perform health activities and clinical neuropsychologist, Dr. Alejandro Fuertes-Saiz, psychiatrist, and Carla Castro, teacher with a specialization in special and curricular education, all professionals from the SINAPSIS Psychology and Speech Therapy center, discuss in this article about transcranial magnetic stimulation and neuropsychological rehabilitation with this stimulation.
The importance of assessment and diagnosis for designing an intervention program
Migraine is a neurological disorder that affects approximately 12% of the world population. Typical symptoms include pulsating headaches, nausea and sensitivity to light and sound.
In addition to these symptoms, migraine can also affect alternating attention and episodic memory. Alternating attention is the ability to shift the focus of attention from one task to another. Meanwhile, episodic memory is the ability to recall specific events and details about those events.
It is crucial in a patient with migraine to perform a neuropsychological assessment to quantify this possible cognitive impairment and develop a comprehensive intervention plan that also addresses these areas.
Neuropsychological rehabilitation with transcranial magnetic stimulation
It is a broader concept than cognitive stimulation, implicing reducing the impact of conditions that are disabling for the client and enabling them to reach an optimal level of social integration (WHO, 2001). Therefore, it includes different types of intervention, which can be grouped into four main categories: cognitive rehabilitation, behavior modification, family intervention and social, educational or vocational reintegration.
Rehabilitation by approach:
- Compensation, consists of the reorganization of functions to minimize or overcome the individual’s functional limitations. Its goal is to improve functionality in daily life. Resources are external aids and environmental adaptations.
- Restoration/Rehabilitation, consists of the direct training of the lost, damaged or deficient function. Its goal is to improve cognitive function through exercises and repetitive tasks of increasing complexity. It implies “bottom-up” mechanisms, where low-level processes pull toward the recovery of high-level processes.
- Substitution, is the construction of a new response method that replaces the damage caused. Its goal is the search for new ways to solve the problem. Resources are the optimization of preserved systems.
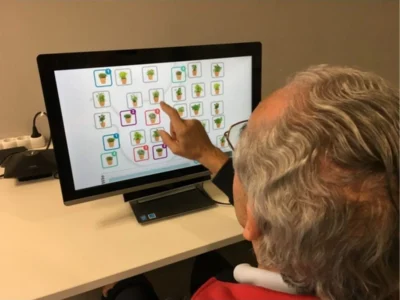
Which neuropsychological processes do we work on through the NeuronUP platform in our case?
Memory is not a unitary system, but there are different memory systems, with distinct contents and related to distinctive brain structures distributed throughout the cerebral cortex. They are systems with an organized brain structure, whose results translate into mental processes and behavior, serving cognitive and behavioral functions.
Tirapu and Grandi published in 2017, in Cuadernos de Neuropsicología, the article “On working memory and declarative memory: proposal for a conceptual clarification”
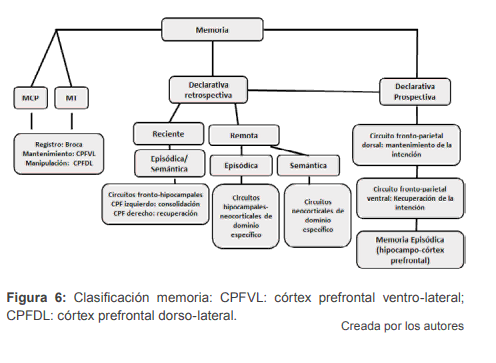
Understanding that episodic memory is the organization of the contents of information subject to spatio-temporal parameters.
Episodic and semantic memory, although representing two declarative memory systems, are anatomically and functionally different. And in turn, taking into account the temporal gradient, we can distinguish retrospective episodic memory (events of the past) or prospective memory (events of the future).
Thanks to our lived experiences, we can organize and plan our future in an adaptive way; examples from our daily life that demonstrate this are reminding yourself to return a book to a friend, taking medication or buying milk at the supermarket.
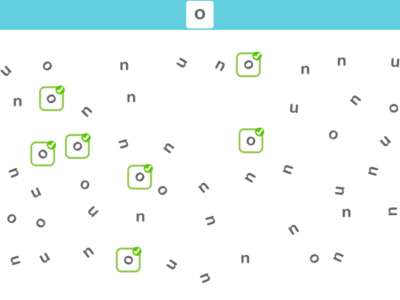
The most commonly used theoretical model when addressing attention is the Sholberg and Mateer clinical model, which establishes five hierarchically ordered levels, with alternating attention being the fourth level.
This means that in order to properly carry out an activity that requires alternating attention, good functioning of the three previous levels is required, that is, focused, sustained and selective attention.
The alternating attention is the ability to change our focus of attention from one task or internal rule to another in a fluid way. For this, the pace at which our brain performs the task is extremely important, that is, our processing speed.
What is non-invasive brain stimulation?
Non-invasive brain neuromodulation techniques are a set of therapeutic tools that seek to modify the electrical activity of certain brain areas to treat various neurological and psychiatric disorders.
These techniques are based on the electrical or magnetic stimulation of the brain, and have become an increasingly popular option due to their efficacy, safety and lack of serious side effects.
Among the most notable techniques we find transcranial magnetic stimulation and transcranial direct current stimulation. Both are painless techniques, with few side effects and growing therapeutic applications in the field of neuropsychiatry (depression, OCD, anxiety, addictions, migraines, post-stroke rehabilitation, etc.)
How does transcranial magnetic stimulation work?
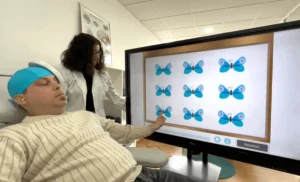
Transcranial magnetic stimulation works by applying magnetic pulses through the scalp (over a cortical target) which induce electric currents in nearby neurons. These electric currents can modify neuronal activity in the stimulated area, either increasing or decreasing it.
The effect of stimulation on brain activity depends on several factors, such as the intensity and frequency of the magnetic pulses, the location of stimulation and the duration of treatment.
In general, it is believed that transcranial magnetic stimulation can increase the activity of neurons in the stimulated area and in connected areas, therefore it has a global effect on the set of brain neurocircuits and not only on the area directly stimulated by the technique.
It has been shown that transcranial magnetic stimulation can increase activity in the dorsolateral prefrontal cortex, a region involved in cognitive and emotional control.
This has led to the exploration of magnetic stimulation as a treatment for depression, anxiety, migraines and other neuropsychiatric disorders that involve dysfunction of the prefrontal cortex.
In summary, transcranial magnetic stimulation is a non-invasive brain neuromodulation technique that works by applying magnetic pulses to modify neuronal activity in specific areas of the brain, which can have therapeutic effects in a variety of neurological and psychiatric disorders.
Advantages of transcranial magnetic stimulation
- No hospitalization required,
- the patient can immediately resume their daily activities,
- no anesthesia required,
- not incompatible with other pharmacological or physical treatments,
- does not produce systemic or serious side effects,
- no prior preparation needed.
Contraindications of transcranial magnetic stimulation
- This technique is not applicable to patients with implanted or non-removable metallic devices in the head (metal plates, cerebrospinal fluid shunt valves, aneurysm clips or coils).
- Treatment with TMS also cannot be used in patients with implants that control physiological signals such as pacemakers, implantable defibrillators, vagus nerve stimulators, spinal cord stimulators or drug infusion pumps.
- Application should be evaluated in patients with epilepsy or a history of seizures.
Side effects of transcranial magnetic stimulation
They are generally mild to moderate and improve shortly after the session and tend to improve as sessions progress. They may include some of the following:
- Headache,
- discomfort in the stimulation area of the scalp,
- tingling sensation, spasms or twitching movements of the facial muscles,
- dizziness,
- 0.003% risk of inducing a seizure.
Case study at the Sinapsis center
Conclusion
Currently, transcranial magnetic stimulation is not only used in approved indications (depression and OCD) but there are numerous promising studies on its application in different pathologies, such as fibromyalgia, spasticity, post-traumatic stress disorder, auditory hallucinations, the negative symptomatology of schizophrenia or stroke rehabilitation.
It should be noted that it should always be used in properly selected cases and when other less costly lines of treatment have failed. The use of transcranial magnetic stimulation as a therapeutic tool in patients with brain damage, whether acquired or degenerative, has increased exponentially in recent years.
Thus, we can find recent research that studies the use of transcranial magnetic stimulation as a therapeutic approach in patients with Parkinson’s disease, Alzheimer-type dementia, traumatic brain injuries, cerebrovascular accidents and other types of neurological, neuropsychological, psychological and psychiatric disorders that present with cognitive impairment as is the case with migraines.
Research conducted to date shows promising results and has demonstrated that transcranial magnetic stimulation is capable of enhancing and inducing neuroplasticity and long-term changes in the brain, both structurally and functionally.
Bibliography
Grandi, Fabrissio & Tirapu, Javier. (2017). On working memory and declarative memory: proposal for a conceptual clarification. Cuadernos de neuropsicología Panamerican Journal of Neuropsychology. 10. 13-31. 10.7714/CNPS/10.3.201.
Ibiricu, M.A. & Morales, G. (2009). Transcranial magnetic stimulation. Anales del Sistema Sanitario de Navarra, 32 (supl.3). Pamplona.
López-Ibor, J.J.; Pastrana, J.I.; Cisneros, S. & López-Ibor, M.I. (2010). Efficacy of transcranial magnetic stimulation in depression. Naturalistic study. Actas Esp. Psiquiatría, 38 (2): 87-93.
Mauro García-Toro, Margalida Gili, Miguel Roca, Chapter 7 – Transcranial magnetic stimulation in psychiatry, Editor(s): Isaac Túnez Fiñana, Álvaro Pascual Leone, Estimulación magnética transcraneal y neuromodulación, Elsevier, 2014, Pages 79-86,
ISBN 9788490224977
Pascual-Leone, A. y Tormos-Muñoz, J.M. (2008). Transcranial magnetic stimulation: foundations and potential for the modulation of specific neural networks. Rev. Neurol., 46 (Supl 1): S3- S10.
If you liked this article about transcranial magnetic stimulation and cognitive rehabilitation, you may also be interested in the following articles:
“This article has been translated. Link to the original article in Spanish:”
La estimulación magnética transcraneal y la rehabilitación cognitiva



 Dementia and Neuropsychological Assessment: The GDS Scale and Its Applicability
Dementia and Neuropsychological Assessment: The GDS Scale and Its Applicability
Leave a Reply