We present a worksheet to work on hemineglect with adults called Comparison of Texts.
What does it involve?
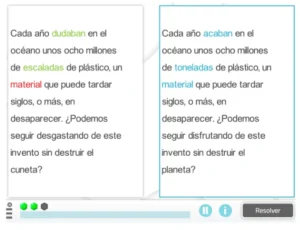
The user must compare two supposedly identical texts and find the words that are different.
The key is to pay close attention since the incorrect words have the same ending as the originals, but their beginning changes. In this way, it forces the person with hemineglect to make an effort to look at the left side of the word, which is where patients with this condition have difficulties.
Play by levels
At the easiest levels it will be easier to find all the words in the text because there will be many fewer than in the advanced levels, where the texts will be much longer.
See in the following video how to play Comparison of Texts 👇
What does this activity work on?
This activity works on several cognitive functions:
Main function
- Hemineglect through comparative reading of texts.
Secondary functions
- Reading,
- Selective attention, since the user must find the incorrect words by comparing both texts.
Paper version
This activity is also available in paper format. The worksheet itself indicates how many errors the user should find.
Research
We created this activity at the request of a research study that is being carried out on NeuronUP and its effectiveness for a specific type of users. Soon you’ll learn more about the research being conducted on our platform! 😉
If you found this post about a worksheet to work on hemineglect with adults useful, you may also be interested in the following:
“This article has been translated. Link to the original article in Spanish:”
Ficha para trabajar la heminegligencia con adultos: Comparación de textos





 Emotional intelligence in schizophrenia: Deficits in schizophrenia
Emotional intelligence in schizophrenia: Deficits in schizophrenia
Leave a Reply