Neuropsychologist Eriz Badiola explains in this article what anosognosia is, what it may be associated with, and what implications it has in day-to-day life.
Anosognosia is often an aspect that is relegated to the background when talking about neuropsychology. Therefore, this article aims to explain what it is, what it may be associated with, and what implications it has in daily life and in clinical practice.
What is anosognosia?
Anosognosia, a neologism derived from the Greek words a (without), nosos (disease) and gnosis (knowledge), would literally be something like “lack of awareness of the disease.” That is, the perspective on certain limitations (cognitive, behavioral, emotional or functional) of the affected person differs from that of others or from the results of objective tests.
This can occur as a consequence of brain lesions resulting from acquired brain injury or neurodegenerative diseases (Mograbi and Morris, 2018).
This difficulty in perceiving limitations can encompass various aspects: from believing they can see when they suffer cortical blindness due to damage in the occipital lobe (Anton-Babinski syndrome), to ignoring that they forget the shopping list, to engaging in behaviors they previously did not perform and, once again, not being aware of it.
Likewise, it should be noted that anosognosia can be partial, so it is possible that the patient is aware of a specific alteration but ignores others, or even minimizes the relevance of the problem.
History of anosognosia
The discovery of this peculiar condition dates back to 1914, when the Franco-Polish neurologist Joseph Babinski (you may also know him for the Babinski sign, the plantar reflex) was working with patients who had suffered strokes in the right hemisphere and consequently suffered a left hemiplegia. In the English translation of the original text by Langer and Levine (2014) it is noted that when one of the patients was asked to raise both arms, she raised the right arm without problem and when it was time to raise the left she either did not answer or said she had raised it. Evidently, she could not raise it, but she believed she had.
Anosodiaphoria
In the 1914 article, our dear Joseph coined the neologism anosognosia; moreover, he added another word to this context: anosodiaphoria (indifference). He used this word to refer to the condition of those patients where the hemiplegia was present, but the importance of the paralysis moved to the background. In other words: being aware of their hemiplegia, they couldn’t have cared less and did not report any distress about it (Langer and Levine, 2014).
Many aspects remained unresolved and from this arose a debate that lasted throughout the past century: does anosognosia really exist or is the patient faking it? Are they denying it?
The debate between anosognosia and denial of the deficit
Our protagonist believed in the existence of anosognosia, although he did not know how to prove it. For him it did not make much sense that a patient would fake for months and months that their arm worked perfectly.
On the other hand, some authors suggest that denial of the deficit can be explained by the psychodynamic paradigm, relating lack of awareness to resistances or defense mechanisms (Ramachandran, 1995; Sims, 2014). However, current neuroscientific perspectives point out that the use of defense mechanisms should be contextualized in patients whose anosognosia does not depend on neurocognitive alterations (Mograbi and Morris, 2018).
Currently, we know that anosognosia is a reality largely of neuropsychological origin and that certain brain lesions can lead to this condition. Moreover, there are neuroanatomical correlates that bring us closer to its understanding.
Neuroanatomical bases of anosognosia and prevalence
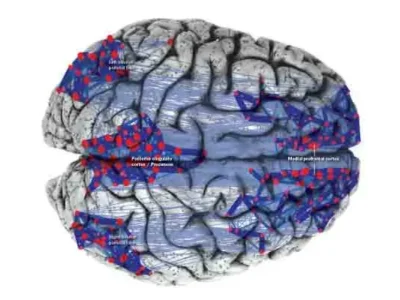
Babinski suggested that anosognosia could be due to lesions in the right hemisphere and that sensory alterations could influence its existence (in fact, patients did not react to external stimuli in those limbs).
Today it would be a mistake to determine that a specific lesion in a precise location can necessarily cause concrete neuropsychological alterations. However, we can say that lesions in certain structures can promote the appearance of such alterations, or lesions in diverse regions can be potentially associated with them.
As mentioned earlier, the etiology of anosognosia is varied, with an incidence between 10 and 18% in patients who have suffered strokes and present with hemiparesis, while up to 81% of people diagnosed with Alzheimer’s are considered to suffer some type of anosognosia and 60% of those with mild cognitive impairment will also experience it (Acharya and Sánchez-Manso, 2018).
In the case of anosognosia for hemiplegia, although it is more frequent in right unilateral or bilateral lesions, the frequency of anosognosia is similar in people with (subcortical and/or cortical) lesions in the temporal, parietal or frontal regions. However, the likelihood of anosognosia is greater in those who suffer lesions both at the frontal and parietal levels, compared to lesions in other brain regions (Pia, Neppi-Modona, Ricci and Berti, 2004).

Subscribe
to our
Newsletter
Anosognosia in mild cognitive impairment
In a recent systematic review (Mondragón, Maurits and De Deyn, 2019) it is noted that in patients with mild cognitive impairment there is a common association between anosognosia and reduced perfusion, as well as activity in the frontal lobe and in midline structures.
Anosognosia in Alzheimer’s disease
Similarly, regarding anosognosia in Alzheimer’s disease, the reviewed studies observe lower perfusion, activation and metabolism in the cortical midline structures, detecting the same phenomenon in parietotemporal structures in more advanced stages of the disease.
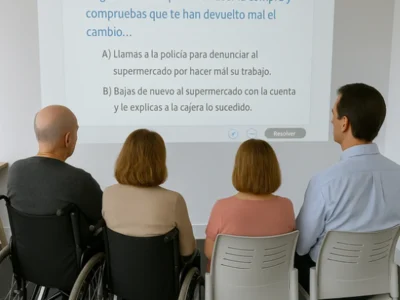
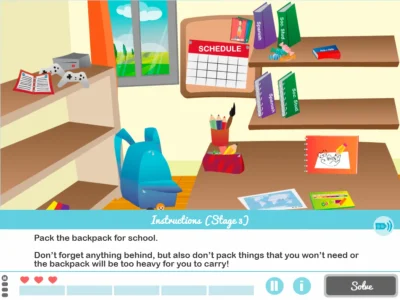
Implications for neuropsychological assessment and rehabilitation
First, in neuropsychological assessment it is possible that given anosognosia, the patient questions the procedure. “Why are you asking me so many questions?” a patient once told me who came to be evaluated to begin neuropsychological rehabilitation after a stroke. Lack of cooperation during assessment could hinder it and confrontation would not always be a solution (even if it seems obvious, I will explain why later). Therefore, and given that the appearance of anosognosia is very diverse, when performing neuropsychological assessment the tests to be administered should be adapted to the individual and unique situation of the patient. Thus, it would be up to the professional’s judgment how to approach the situation with the skills they acquire through experience.
Another situation that may occur during rehabilitation sessions is that a patient with memory problems (for example, people with Alzheimer’s) ignores the existence of memory deficits, with a greater probability of anosognosia the more advanced the disease is (Hanseew et al., 2019). What happens with anosognosia associated with memory problems and the people who suffer from it (especially episodic memory) is that no matter how much the patient is confronted about the existence of such difficulties, it is not productive, because they will feel worse and will probably not remember what happened by the next session. In this regard, I recommend watching “When and how to address anosognosia?”, a video where the approach for people with Alzheimer’s and for those who suffer acquired brain injury is differentiated (Ruiz-Sánchez de León, 2020).
For all these reasons, we must not forget to inform and educate family members and caregivers, so that they take anosognosia into account, as it can be a source of conflicts where both the patient and the family member may feel bad. In this context, two considerable pillars for addressing this situation are: understanding and empathy. From both the family members and the clinical neuropsychologist.
In summary, anosognosia is a faithful companion to acquired brain injury and neurodegenerative diseases, which we must take into account both in assessment and in neuropsychological rehabilitation. The approach must be adapted to the patient and considered from a multidisciplinary perspective. Likewise, family members should be included and made participants on the path toward improving the quality of life of the people we want to help.
Bibliography
- Acharya, A. B., and Sánchez-Manso, J. C. (2018). Anosognosia. StatPearls Publishing: Treasure Island (Florida).
- Hanseeuw, B. J., Scott, M. R., Sikkes, S. A., Properzi, M., Gatchel, J. R., Salmon, E., … and Alzheimer’s Disease Neuroimaging Initiative. (2020). Evolution of anosognosia in alzheimer’s disease and its relationship to amyloid. Annals of neurology, 87(2), 267-280.
- Langer, K. G., and Levine, D. N. (2014). Babinski, J. (1914). Contribution to the study of the mental disorders in hemiplegia of organic cerebral origin (anosognosia). Translated by K.G. Langer & D.N. Levine. Translated from the original Contribution à l’Étude des Troubles Mentaux dans l’Hémiplégie Organique Cérébrale (Anosognosie). Cortex; a journal devoted to the study of the nervous system and behavior, 61, 5–8.
- Mondragón, J. D., Maurits, N. M., and De Deyn, P. P. (2019). Functional neural correlates of anosognosia in mild cognitive impairment and alzheimer’s disease: a systematic review. Neuropsychology review, 29(2), 139-165.
- Mograbi, D. C., and Morris, R. G. (2018). Anosognosia. Cortex; a journal devoted to the study of the nervous system and behavior, 103, 385-386.
- Pia, L., Neppi-Modona, M., Ricci, R., & Berti, A. (2004). The anatomy of anosognosia for hemiplegia: a meta-analysis. Cortex, 40(2), 367-377.
- Ruiz-Sánchez de León, J.M. [LOGICORTEX Neuropsicología]. (2020, September 2). When and how to address anosognosia? [Video file]. Retrieved from https://www.youtube.com/watch?v=uJi7_v_CluM
- Ramachandran, V. S. (1995). Anosognosia in parietal lobe syndrome. Consciousness and cognition, 4(1), 22-51.
- Sims, A. (2014). Anosognosia and the very idea of psychodynamic neuroscience (No. Ph. D.). Deakin University.
More Recommended Reading
- Orfei, M. D., Caltagirone, C., and Spalletta, G. (2009). The evaluation of anosognosia in stroke patients. Cerebrovascular diseases, 27(3), 280-289.
- Starkstein, S. E. (2014). Anosognosia in Alzheimer’s disease: diagnosis, frequency, mechanism and clinical correlates. Cortex, 61, 64-73.
If you liked this article about anosognosia, you may also be interested in these other posts:
“This article has been translated. Link to the original article in Spanish:”
Anosognosia: qué es, historia y realidad neuropsicológica


 Neuroeducation: neuroscience applied to school learning
Neuroeducation: neuroscience applied to school learning
Leave a Reply