The study of consciousness remains a mystery for contemporary science. However, it is increasingly becoming a key factor in the recovery of patients who have suffered an acquired brain injury. Many therapeutic neuropsychological rehabilitation processes fail because they cannot count on the patient’s collaboration, since they do not adhere to prescribed guidelines, refuse to undergo group rehabilitation sessions, or do not attend scheduled appointments. This does not occur from a lack of will or understanding, but is part of a neuropsychological alteration that makes the patient not perceive their deficit and act as if everything were fine.
What is consciousness?
Consciousness is an extremely complex construct. If today we do not have a single, unambiguous definition of this mental function, it is probably due to its extraordinary ubiquity in the brain and its multifaceted nature. The British philosopher John Locke (1632-1704) defined consciousness as the “perception of what goes on in one’s own mind.” More modern definitions maintain that consciousness is characterized as “a mental state that is private, personal, subjective, and qualitative, which integrates in a unitary, coherent, and continuous way multiple personal experiences (qualia).”
Differences between being conscious and being aware
A useful distinction is the one made in Spanish between ‘estar consciente’ and ‘ser consciente’. Estar consciente would be the same as being awake and alert, receptive to environmental stimuli, so that consciousness from this point of view would be what one has when awake and what one loses when deeply asleep or under anesthesia. On the other hand, ser consciente would be more related to the human capacity to know one’s own thought and to objectively understand the world and oneself, while at the same time maintaining a sense of subjectivity.
These properties of consciousness would have an identifiable neuroanatomical basis in the brain, although knowledge about their neuronal localization is still frankly uncertain. To be awake we need activation and alertness, basic functions that would depend on structures in the brainstem, the ascending reticular activating system (S.A.R.A.), and fronto-parietal noradrenergic circuits, lateralized to the right hemisphere when we speak specifically of arousal. The ability to focus the spotlight of attention on a particular perception would depend on posterior parietal areas and some thalamic nuclei such as the pulvinar. The generation of conscious experiences has been related to reverberant cortico-thalamic circuits, consistently in bands of synchronized neuronal discharges at 40 hertz. Finally, self-awareness, that is, the substrate of reflection about oneself, identity and theory of mind, would be located in the prefrontal cortex.
Therefore, as we can see, consciousness is not a unitary construct. Indeed, as was already distinguished in philosophy, there are different types of consciousness with different neuroanatomical bases, which help generate the conscious and self-aware experiences we have in our daily lives.

Lack of awareness of deficits: anosognosia
One of the things that most surprises the novice neuropsychologist is the lack of awareness of deficits in patients with acquired brain injury. Patients with Wernicke’s aphasia who believe they speak coherently and are understood, patients with hemineglect who bump into doors or do not eat food located on the contralateral side of the plate, patients with severe problems of emotional self-regulation and insight after a frontal lobe injury who deny any kind of problem, are common cases in neuropsychology clinics. All of them pose a challenge for the clinician both in assessment and in treatment planning.
What is anosognosia?
The term anosognosia was first introduced by the French neurologist Charles Babinski in 1914 when he reported a case of hemiplegia in which the patient had no awareness of his deficit. Subsequently, the term ‘anosognosia’ has become popularized and extended to refer, in general, to the absence of awareness of deficits, whether these are physical, cognitive, emotional, interpersonal, or of personality.
Anosognosia or lack of awareness of deficits is an alteration frequently observed in patients who have suffered brain injury, whether traumatic, from cerebrovascular accident, neoplastic or infectious. Its prevalence, according to various studies, ranges between 33% and 52%. In addition, around half still present this alteration one year after suffering an acquired brain injury. Its presence constitutes a poor prognostic factor, as it usually translates into lack of motivation, low treatment adherence, poor participation in scheduled activities and mismatches between the patient’s expectations of their own ability and the reality.
Therapeutic approach to lack of awareness of deficits in acquired brain injury
When planning a neuropsychological intervention program it is recommended to follow a series of principles that will help us design the best possible intervention adapted to the specific needs of our patient. For this, we should start from theoretical reference models that allow us to interpret the results obtained in tests, adopt an interdisciplinary and multiple perspective and focus rehabilitation more on disability than on deficits. This usually implies conducting an exhaustive analysis of the functional consequences that the acquired brain injury has had on the patient’s life and trying to achieve the greatest possible social and occupational adaptation.
Lack of awareness of deficits can produce marked interference in the daily lives of people who suffer a neuropsychological disorder. Likewise, it can hinder adherence to rehabilitation sessions. Therefore, the therapeutic approach to lack of awareness of deficits in the context of acquired brain injury, if present, becomes the first therapeutic target that the neuropsychologist must take into account in treatment planning.
Most intervention programs developed to improve awareness of deficits have common objectives focused on increasing the patient’s knowledge of the lesion, working on acceptance of their limitations and reducing the mismatch between their expectations of functioning and actual performance. In addition, establishing a good therapeutic alliance is fundamental in this process, especially if by increasing awareness of deficits the patient begins to show depressive symptoms, anxiety or even denial.

Subscribe
to our
Newsletter
Intervention strategies for rehabilitating awareness of deficits in acquired brain injury
In a recent systematic review, Villalobos and colleagues (2020) set out the intervention strategies most commonly used in the rehabilitation of awareness of deficits in acquired brain injury: psychoeducation, feedback, confrontation, behavioral therapy and psychotherapy.
Psychoeducation
Through psychoeducation, information adapted to the patient’s capacity for understanding is offered about the nature of their disorder, the associated deficits and the functional repercussions it produces, with the aim of increasing their knowledge about their problem.
Feedback
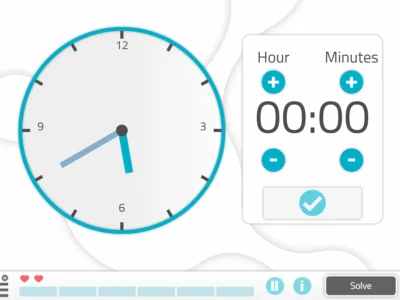
The aim of feedback is to inform the patient about their performance on a specific task. This will allow them to know whether they are reaching the goal or how far they are from it, so they can adjust their performance or seek appropriate strategies to achieve it.
Confrontation
Confrontation is used to measure the mismatch between the patient’s expectations and their actual performance on a task. For this purpose, structured tasks are designed that allow for self-monitoring and self-evaluation, always starting from the patient’s current capacities at that moment. The patient must make a prediction about their performance on the task before performing it and then analyze and compare it with the result obtained. The experiential trial usually has a great impact on the knowledge patients have of their new reality. Therefore, it is necessary to proceed with caution and carefully evaluate the pros and cons of this type of intervention, as well as choose the most appropriate moment within the rehabilitation process of the acquired brain injury.
Behavioral therapy
Precisely when we suspect that confrontation may produce anxiety or be psychologically harmful for the patient, it is advisable to begin with training in compensatory strategies as well as work on acquiring procedural habits that allow the patient to gain functionality.
Psychotherapy
Psychotherapy can be useful at different stages of recovery from acquired brain injury, especially when it involves lack of awareness of deficits. In the scientific community, controversy surrounds the etiology of anosognosia, which could have a neurological origin, but also a psychological one, through mechanisms of denial. In any case, psychotherapy can be useful both to help the patient manage the emotional disturbances that this type of disorder entails, and to restore a new sense in their life, as well as to outline new goals adjusted to their new reality.
Conclusions about awareness of deficits as a key factor in recovery from acquired brain injury
The therapeutic approach to lack of awareness of deficits is attracting growing interest among both researchers and neuropsychologists. As we have seen, rehabilitating a cognitive, emotional or behavioral alteration after an acquired brain injury can be much more difficult if the patient is not aware of their deficit. Numerous studies have highlighted the predictive value of lack of awareness of deficits for the reintegration of patients affected by acquired brain injury. In fact, the less awareness of the deficit, the worse the reintegration.
For this reason, the development of new theoretical models, measurement instruments and rehabilitation programs that allow us to continue advancing in order to offer patients the best therapeutic tools adapted to their disorder is increasingly necessary. It is evident that, in some way, we already work on these aspects with patients, but this must be done in a more systematic and structured way. Only in this way will we be able to improve knowledge about the processes of monitoring consciousness and contribute to developing an evidence-based neuropsychology.
References on acquired brain injury and awareness of deficits
- Adolphs, R. (2015). The unsolved problems of neuroscience. Trends in Cognitive Science, 19(4) 173-75.
- Aznar-Casanova, J.A. (2017). Consciousness: the polynomic interface of subjectivity. Madrid: Pirámide.
- Locke, J. (1690/1980). An Essay Concerning Human Understanding. Editora Nacional, Madrid.
- Flashman, L. A. & McAllister, T.W. (2002). Lack of awareness and its imact in traumatic brain injury. Neurorrehabilitation, 17(4), 185-96.
- Graziano, M. (2015). Consciousness and the social brain. New York: Oxford University Press.
- González, B., Paúl, N., Blázquez, J. L. & Ríos, M. (2006). Factors related to lack of awareness of deficits in brain injury. Acción Psicológica, 4(3), 87-99.
- Muñoz-Céspedes, J.M. & Tirapu-Ustárroz, J. (2001). Neuropsychological rehabilitation. Madrid: Síntesis
- Robertson, K. & Schmitter-Edgecombe, M. (2015). Self-awareness and traumatic brain injury outcome, Brain Injury, 29:7-8, 848-858, DOI: 10.3109/02699052.2015.1005135.
- Tirapu-Ustárroz, J. (2008). What is the brain for? Bilbao: Desclée de Brouwer.
- Villalobos, D., Bilbao, A., López-Muñoz, F. & Pacios, J. (2020). Awareness of deficit as a key process in the rehabilitation of patients with acquired brain injury: systematic review. Revista de Neurología, 70(1), 1-11.
If you liked this post about awareness of deficits in the recovery from acquired brain injury, you might be interested in these publications from NeuronUP:
“This article has been translated. Link to the original article in Spanish:”
La consciencia de los déficits en la recuperación del daño cerebral adquirido






 The advantages of working with NeuronUP in pediatric and adolescent populations
The advantages of working with NeuronUP in pediatric and adolescent populations
Leave a Reply